Multi-lesion, left-sided, single isocenter radiosurgery treatment in a patient with a pacemaker
Images
CASE SUMMARY
An 85-year-old male with a history of ventricular arrhythmia requiring an automatic implantable cardioverter/defibrillator (AICD), and a T2N0M0 basaloid squamous cell carcinoma of the base of tongue treated with definitive cetuximab and external-beam radiotherapy to 70.2 Gy 2-and-a-half years prior, was referred to our department after his AICD fired and triggered a workup by his primary care physician (PCP). An initial chest x-ray revealed new pulmonary opacities, prompting a CT of the chest, which showed 4 left-sided pulmonary lesions as well as 1 right-sided pulmonary lesion. Pathology from a CT-guided biopsy was consistent with his primary basaloid squamous cell carcinoma from the base of tongue. Due to his multiple comorbidities, chemotherapy was an ill-advised option. The physical exam was unrevealing.
IMAGING FINDINGS
Preoperative magnetic resonance imaA PET/CT scan revealed 4 hypermetabolic lesions within the left lung, measuring from 2.2-×-2.8 cm in diameter with SUVmax values of 11.6 to 15.4. There was also a right-sided paraesophageal mass measuring 1.4-×-2.4 cm with an SUVmax of 10.4 and no further evidence of metastatic disease.
DIAGNOSIS
The patient was diagnosed with oligometastatic basaloid squamous cell carcinoma from his base of tongue primary.
DISCUSSION
As a result of this entity’s rarity, stereotactic radiosurgery (SRS) has become the standard of care in treating small pulmonary lesions, both primary and metastatic, in the medically inoperable population.1 More recently, it has been used in patients with so-called oligometastatic disease. Oligometastases are isolated tumor deposits that appear to have a different natural history from widespread metastatic disease.2 When treated adequately, patients with oligometastatic disease can have significant local control of their tumor deposits with an apparent increase in expected overall and progression-free survival.3,4
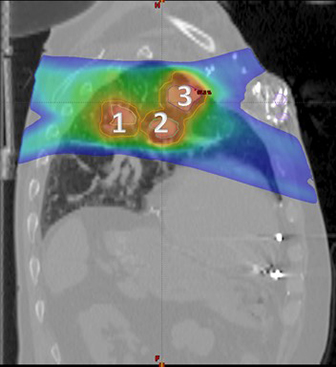
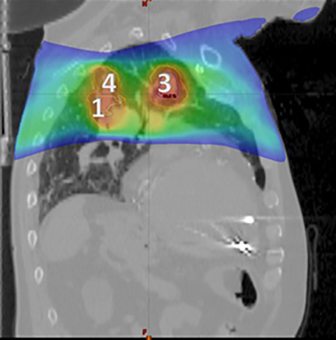
Typically, oligometastatic lesions would be treated sequentially if spatially disparate, or at the very least, each with their own unique isocentric plans. In this particular patient, however, his 4 left-sided lesions were arranged in a configuration such that we were able to use 1 isocenter and treat all 4 simultaneously (Figures 1 and 2).
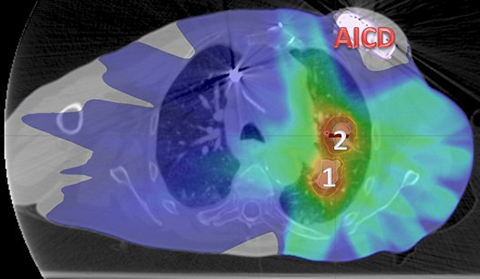
Furthermore, his AICD provided a unique challenge in the planning phase (Figure 3). As most devices have a recommended dose tolerance of 2Gy5 and our plan was to deliver a total dose of 48Gy in 4 fractions to his lesions, his plan required deft beam arrangements to avoid overdosing his AICD. The motion of each lesion within a common gating window was assessed individually and taken into account when creating the PTVs, and a pre-treatment cone-beam CT was used to ensure alignment. Twelve beams were used for treatment delivery. Upon a physics evaluation, it was estimated that his pacemaker would receive approximately 20 cGy per fraction, totaling 80 cGy throughout the course of treatment, a dose well below the tolerance of his device.
Each treatment required approximately 45 minutes. He completed treatment without incident and went on to have his right para-esophageal lesion treated with SRS as well. At his 6-month follow up, a PET/CT scan indicated that he had no residual activity in any of the 5 lesions. Interestingly, he had no further AICD firing events.
CONCLUSION
To date, there have been no reports of multi-lesion, single isocenter SRS treatments for extra-cranial disease. The technique has been used, however, for multiple intracranial lesions with excellent results.6,7 Extrapolating from the central nervous system (CNS) model, we were able to achieve a treatment plan for our patient’s 4 left-sided oligometastases that used a single isocenter. This is a critical achievement for a number of reasons. By using a single (as opposed to multiple) isocenter, we were able to treat this patient in a 45-minute time slot. A multi-centric treatment plan would require treatment times proportional to the number of lesions being irradiated: Each lesion may require table shifts and verification in addition to beam-on time. Reducing time-on-table is important not only for patient comfort and satisfaction, but it may also be related to clinical outcomes and is under investigation at our institution. Additionally, in an environment where growing healthcare costs are always of concern, unicentric plans are less expensive than multicentric plans as a result of fewer dosimetric and physics charges.
REFERENCES
- Timmerman R, Paulus R, Galvin J. Stereotactic body radiation therapy for inoperable early stage lung cancer. JAMA. 2010;303(11). Available at: http://archpsyc.jamanetwork.com/article.aspx?articleid=185547. Accessed July 31, 2014.
- Mehta N, Mauer AM, Hellman S, et al. Analysis of further disease progression in metastatic non-small cell lung cancer: Implications for locoregional treatment. Int J Oncol. 2004;25(6):1677-83. Available at: http://www.ncbi.nlm.nih.gov/pubmed/15547705. Accessed August 4, 2014.
- Milano MT, Philip A, Okunieff P. Analysis of patients with oligometastases undergoing two or more curative-intent stereotactic radiotherapy courses. Int J Radiat Oncol Biol Phys. 2009;73(3):832-7. doi:10.1016/j.ijrobp.2008.04.073.
- Parikh RB, Cronin AM, Kozono DE, et al. Definitive primary therapy in patients presenting with oligometastatic non-small cell lung cancer. Int J Radiat Oncol Biol Phys. 2014;89(4):880-7. doi:10.1016/j.ijrobp.2014.04.007.
- Marbach JR, Sontag MR, Van Dyk J, Wolbarst AB. Management of radiation oncology patients with implanted cardiac pacemakers: report of AAPM Task Group No. 34. American Association of Physicists in Medicine. Med Phys. 1994;21(1):85-90. Available at: http://www.ncbi.nlm.nih.gov/pubmed/8164594. Accessed August 22, 2014.
- Huang Y, Chin K, Robbins JR, et al. Radiosurgery of multiple brain metastases with single-isocenter dynamic conformal arcs (SIDCA). Radiother Oncol. 2014. doi:10.1016/j.radonc.2014.05.009.
- Clark GM, Popple RA, Prendergast BM, et al. Plan quality and treatment planning technique for single isocenter cranial radiosurgery with volumetric modulated arc therapy. Pract Radiat Oncol. 2012;2(4):306-13. doi:10.1016/j.prro.2011.12.003.