Adapting to the Virtual World: An Analysis of Remote Work Policies in Academic Radiation Oncology
Affiliations
- Medical College of Wisconsin, Milwaukee, WI
- State University of New York (SUNY) Upstate Medical University, Syracuse, NY
- Oregon Health Sciences University, Portland, OR
- University of California San Francisco, San Francisco, CA
- MD Anderson Cancer Center, Houston, TX
- University of Washington, Seattle, WA
- Virginia Garcia Memorial Health Center and Foundation, Newburgh, OR
- Veteran Affairs New York Harbor Healthcare System, SUNY - Downstate Medical Center, New York, NY
- Emory University, Atlanta, GA
- Massachusetts General Hospital, Exeter, NH
- Arizona Center for Cancer Care, Scottsdale, AZ
- Yale School of Medicine, New Haven, CT
- Kaiser Permanente, Portland, OR.
†Dr. Beltran Ponce and Ms. LoTemplio are co-first authors and contributed equally to the work
*Corresponding Author: Amy LoTemplio, BA, 509 Columbus Ave, Apt. 2., Syracuse, NY 13210 lotempla@upstate.edu
Abstract
Objective:
The COVID-19 pandemic led to a shift from traditional work environments to working from home (WFH). The specific benefits and challenges of WFH in radiation oncology (RO) are currently unknown. To address this gap in knowledge, a survey-based study was conducted to assess WFH policies and perceptions of their impact, as well as explore the role of departmental gender composition in remote work policies.
Materials and Methods:
Faculty and residents were randomly selected from the 92 American College of Graduate Medical Education-accredited RO residency programs. Descriptive statistics were generated for responses overall and separately among faculty and residents for demographic responses. They were also generated for responses relating to remote policy among departments with at least one-third female faculty/residents and those with less than one-third female faculty/residents. Associations between responses and groups were assessed using chi-square or Fisher exact tests for categorical responses and Wilcoxon rank-sum tests for numerical responses.
Results:
Although 58.6% of faculty and 59.1% of residents perceived a negative or somewhat negative impact of WFH on patient satisfaction, the majority (> 51%) had positive perceptions of impact on all other measured outcomes, including their time with children, time with partner, time with other family members, and their personal wellness. Additionally, the current study revealed that 93.4% (n = 57) of departments comprised of more than one-third women had WFH policies in place, while only 84.2% (n = 64) of departments comprised of fewer than one-third female members had such policies.
Conclusion:
These findings highlight the importance of diverse input from all genders as departments implement WFH policies. Further research should explore the durability of changes in workplace flexibility and how they may impact gender disparities within RO.
Keywords
work from home, academic radiation oncology, gender disparitiesIntroduction
The COVID-19 pandemic has led to a significant shift from traditional work environments to working from home (WFH) for many health care workers.1 - 3 This transition significantly impacted individuals responsible for family care as school closures required caretakers to balance professional, domestic, and educational roles.1 These demands disproportionately impact women, who typically bear a greater portion of domestic and childcare responsibilities.4
This holds true in academic medicine, where women have been negatively impacted.5 , 6 First-author publications by women decreased in the first year of the pandemic, despite a 2020 survey reporting that 41% of women felt they were expected to be more productive throughout COVID-19.5 , 6 For instance, when compared with papers published in 2019, Andersen et al found that papers published between January 1, 2020 and May 5, 2020 had 23%, 16% and 16% lower proportion of female first authors, last authors, and general authors, respectively.5 The misalignment between expectation and reality has placed a burden on women in academic medicine.
Before the pandemic, only 52% of female radiation oncology (RO) residents felt RO was family-friendly, and only 5% reported no symptoms of burnout.7 Since COVID-19, female physicians have reported high levels of career uncertainty, and 71% of physician mothers with young children reported feeling that the pandemic limited their career advancement.6
Because little is known about how RO departments implemented WFH policies and how these policies were perceived in the field, we conducted a study to investigate the implementation of WFH policies in RO and explore the role that departmental gender composition played in the development of remote work policies. These understandings may aid in the design of equitable remote work policies beyond COVID-19.
Materials and Methods
This is a survey-based analysis that seeks to describe WFH policies within RO, perceptions of their impact, and whether the gender composition of departments was associated with policy characteristics. The questions of the survey were written by members of the Society for Women in Radiation Oncology (SWRO) and reviewed by the executive committee of SWRO and some members of the senior advisory counsel. The study received institutional review board (IRB) approval.
Study Sample and Survey Administration
The survey was administered to the RO program director and 1 randomly selected resident from each US academic RO department. These participants were invited to complete an anonymous, web-based survey distributed through RedCap to all 92 American College of Graduate Medical Education-accredited RO residency programs in the United States. If the contacted RO program director or resident did not respond, a random faculty member or resident was chosen. Responses were collected from December 2020 to February 2021, with reminders sent every 2 weeks. If no response was received after the second reminder, an alternate participant was selected from the same institution.
Survey Development and Measures
The survey consisted of 32 questions and assessed 5 themes: (1) respondent/department demographics, (2) WFH departmental policies, (3) perceived impact of WFH policies on domains of work and personal life, (4) utilization of WFH policy, and (5) sentiments about WFH. The survey assessed domains such as children’s education, personal wellness, and time with family, as well as work-related tasks, patient care, educational responsibilities, research duties, and leadership duties. Data were held in RedCap and analyzed using R.
Statistical Analysis
Descriptive statistics were generated for overall responses. For demographic questions, responses were stratified by the responder’s role. For questions relating to remote policy, departments were stratified by those with at least one-third female faculty or residents and those with less than one-third female faculty or residents.
Associations between multiple-choice responses and stratification variables were assessed using Fisher exact tests when the expected value for any response subgroup was less than 5; in other cases, Pearson‘s chi-square tests were used. For the numerical response, a Wilcoxon rank-sum test was used.
All analyses were performed using R (version 4.0.5) and RStudio (version 1.4.1103) software.
Results
A total of 146 responses were collected from 77 departments (84% of those contacted). Among the 77 faculty and 69 residents surveyed, 55% identified as female, 58% were White, and 51% were between 31 and 40 years, an age when most residents start to consider having families ( Table 1 ). Of the represented departments, 45% (n = 61) reported having less than one-third female-identifying faculty/residents. Among respondents, 48% reported that a majority or almost all males in their program had children or other vulnerable dependents in the household, while 44% responded this way regarding female colleagues. Before the pandemic, 6.8% (n = 10) of faculty and 9.1% (n = 7) of residents reported feeling responsible for child education. These values increased to 14% (n= 21) and 21% (n = 16), respectively, during the pandemic.
Survey of Participant Demographics
| OVERALL n = 146) | FACULTY (n = 77) | RESIDENT (n= 69) | P VALUE* | |
|---|---|---|---|---|
| Age [n (%)] | < .001 | |||
| 21-30 | 27 (18%) | 1 (1.3%) | 26 (38%) | |
| 31-40 | 74 (51%) | 33 (43%) | 41 (59%) | |
| 41-50 | 29 (20%) | 27 (35%) | 2 (2.9%) | |
| 51-60 | 11 (7.5%) | 11 (14%) | 0 (0%) | |
| > 60 | 5 (3.4%) | 5 (6.5%) | 0 (0%) | |
| Gender [n (%)] | < .001 | |||
| Female | 80 (55%) | 57 (74%) | 23 (33%) | |
| Male | 66 (45%) | 20 (26%) | 46 (67%) | |
| Race/ethnicity [n (%)] | .2 | |||
| Asian | 43 (29%) | 24 (31%) | 19 (28%) | |
| Black or African American | 1 (.7%) | 1 (1.3%) | 0 (0%) | |
| Hispanic, Latino, or Spanish origin | 8 (5.5%) | 7 (9.1%) | 1 (1.4%) | |
| White or Caucasian | 85 (58%) | 39 (51%) | 46 (67%) | |
| Other | 3 (2.1%) | 2 (2.6%) | 1 (1.4%) | |
| Prefer not to answer | 6 (4.1%) | 4 (5.2%) | 2 (2.9%) | |
| Program location [n (%)] | .7 | |||
| New England | 7 (5.0%) | 5 (6.8%) | 2 (3.0%) | |
| Middle Atlantic | 26 (19%) | 12 (16%) | 14 (21%) | |
| East North Central | 27 (19%) | 12 (16%) | 15 (22%) | |
| West North Central | 9 (6.4%) | 3 (4.1%) | 6 (9.0%) | |
| South Atlantic | 25 (18%) | 14 (19%) | 11 (16%) | |
| East South Central | 11 (7.9%) | 5 (6.8%) | 6 (9.0%) | |
| West South Central | 10 (7.1%) | 6 (8.2%) | 4 (6.0%) | |
| Mountain | 6 (4.3%) | 3 (4.1%) | 3 (4.5%) | |
| Pacific | 19 (14%) | 13 (18%) | 6 (9.0%) | |
| Not provided | 6 | 4 | 2 | |
| Population where located [n (%)] | .4 | |||
| < 2500 | 1 (.7%) | 1 (1.4%) | 0 (0%) | |
| > 20,000 | 14 (10%) | 8 (11%) | 6 (9.0%) | |
| < 250,000 | 7 (5.0%) | 5 (6.8%) | 2 (3.0%) | |
| 250,000-1,000,000 | 37 (26%) | 15 (21%) | 22 (33%) | |
| > 1,000,000 | 81 (58%) | 44 (60%) | 37 (55%) | |
| Not provided | 6 | 4 | 2 | |
| Number of faculty/residents [median (IQR)] | 9 (7, 14) | 12 (8, 20) | 8 (6, 11) | < .001 |
| Not provided | 9 | 6 | 3 | |
| Faculty/resident demographics | .2 | |||
| At least one-third female | 61 (45%) | 35 (49%) | 26 (39%) | |
| Less than one-third female | 76 (55%) | 36 (51%) | 40 (61%) | |
| Not provided | 9 | 6 | 3 | |
| Percent with children and/or dependents (female) [ n (%)] | < .001 | |||
| Few (< 10%) | 44 (32%) | 6 (8.3%) | 38 (58%) | |
| Minority (10-50%) | 21 (15%) | 9 (12%) | 12 (18%) | |
| Majority (50-80%) | 24 (17%) | 19 (26%) | 5 (7.6%) | |
| Almost all (> 90%) | 37 (27%) | 32 (44%) | 5 (7.6%) | |
| I don't know | 12 (8.7%) | 6 (8.3%) | 6 (9.1%) | |
| Not provided | 8 | 5 | 3 | |
| Percent with children and/or dependents (male) [n (%)] | < .001 | |||
| Few (< 10%) | 17 (12%) | 0 (0%) | 17 (26%) | |
| Minority (10-50%) | 45 (33%) | 10 (14%) | 35 (53%) | |
| Majority (50-80%) | 39 (28%) | 27 (38%) | 12 (18%) | |
| Almost all (> 90%) | 27 (20%) | 26 (36%) | 1 (1.5%) | |
| I don't know | 10 (7.2%) | 9 (12%) | 1 (1.5%) | |
| Not provided | 8 | 5 | 3 | |
| Responsibilities prior to the pandemic [n (%)] | ||||
| Childcare | 19 (13%) | 14 (18%) | 5 (7.2%) | .05 |
| Child education | 10 (6.8%) | 7 (9.1%) | 3 (4.3%) | .3 |
| Other dependent care | 9 (6.2%) | 6 (7.8%) | 3 (4.3%) | .5 |
| Responsibilities at the onset of the pandemic [n (%)] | ||||
| Childcare | 23 (16%) | 16 (21%) | 7 (10%) | .078 |
| Child education | 21 (14%) | 16 (21%) | 5 (7.2%) | .02 |
| Other dependent care | 10 (6.8%) | 7 (9.1%) | 3 (4.3%) | .3 |
*Pearson’s chi-square test or Fisher exact test for categorical variables; Wilcoxon rank-sum test for number of faculty/residents.
Only one department reported having a WFH policy in place before the pandemic ( Table 2 ), while 42% reported having an ongoing WFH policy. Of those departments with WFH policies, 78% reported that policy installments were within the first 1-2 months of the onset of the pandemic. Of the departments comprised of at least one-third female members, 93.4% (n = 57) had WFH policies in place, while only 84.2% (n = 64) of the departments comprised of fewer than one-third female members had WFH policies in place. Of the departments with a WFH policy during the initial phase of the pandemic, most later reduced their WFH allowances (56%, n = 68), while 12% (n = 15) expanded and 31% (n = 38) left them unchanged. In departments with less than one-third female faculty, 18% (n = 8) had policies that allowed for moderate (2-3 d at home) or full remote work policy options while 36% (n= 14) of the departments with at least one-third female faculty members had such policies. Table 2 provides further details regarding the extent of WFH, rationale for its implementation, and tasks included in WFH provisions.
Participant Responses Relating to Questions About Their Remote Work Policy
| OVERALL (n = 137) | AT LEAST ONE-THIRD FEMALE (n = 61) | LESS THAN ONE-THIRD FEMALE (n = 76) | P VALUE* | |
|---|---|---|---|---|
| Presence of policy [n (%)] | .15 | |||
| Remote work policy already in place prior to the pandemic | 1 (.7%) | 1 (1.6%) | 0 (0%) | |
| Remote work policy started during the pandemic, ongoing | 57 (42%) | 24 (39%) | 33 (43%) | |
| Remote work policy started during the pandemic, now modified | 63 (46%) | 32 (52%) | 31 (41%) | |
| No remote work policy | 16 (12%) | 4 (6.6%) | 12 (16%) | |
| When policy started [n (%)] | .4 | |||
| Within the first 1-2 mo of the onset of the US pandemic (January-March) | 94 (78%) | 42 (75%) | 52 (81%) | |
| 3-4 mo after the start of the US pandemic (April-May) | 25 (21%) | 14 (25%) | 11 (17%) | |
| June 2020 or thereafter | 1 (.8%) | 0 (0%) | 1 (1.6%) | |
| No response | 17 | 5 | 12 | |
| How policy has changed [n (%)] | .9 | |||
| Expanded | 15 (12%) | 8 (14%) | 7 (11%) | |
| Contracted | 68 (56%) | 31 (54%) | 37 (58%) | |
| Unchanged | 38 (31%) | 18 (32%) | 20 (31%) | |
| No response | 16 | 4 | 12 | |
| Amount of remote work (initial) [n (%)] | .9 | |||
| Minimal remote work options (1 d per week at home) | 43 (36%) | 19 (33%) | 24 (38%) | |
| Moderate remote work options (2-3 d at home) | 59 (49%) | 29 (51%) | 30 (47%) | |
| Full remote work capability (all remote with only necessary in person interaction) | 19 (16%) | 9 (16%) | 10 (16%) | |
| No response | 16 | 4 | 12 | |
| Amount of remote work (current) [n (%)] | .056 | |||
| No remote work | 22 (27%) | 12 (31%) | 10 (23%) | |
| Minimal remote work options (1 d per week at home) | 34 (41%) | 10 (26%) | 24 (55%) | |
| Moderate remote work options (2-3 d at home) | 20 (24%) | 12 (31%) | 8 (18%) | |
| Full remote work capability (all remote with only necessary in person interaction) | 2 (2.4%) | 2 (5.1%) | 0 (0%) | |
| Other | 5 (6.0%) | 3 (7.7%) | 2 (4.5%) | |
| No response | 54 | 22 | 32 |
| OVERALL (n = 121) | AT LEAST ONE-THIRD FEMALE (n= 57) | LESS THAN ONE-THIRD FEMALE (n = 64) | P VALUE* | |
|---|---|---|---|---|
| Department rationale for policy [n (%)] | ||||
| Public health (prevalence and risk of COVID-19 in the community) | 118 (98%) | 55 (96%) | 63 (98%) | .6 |
| Culture (preference spoken by physicians) | 25 (21%) | 13 (23%) | 12 (19%) | .6 |
| Financial (dependents at home) | 14 (12%) | 11 (19%) | 3 (4.7%) | .012 |
| Legal | 1 (.8%) | 0 (0%) | 1 (1.6%) | > .9 |
| Other | 3 (2.5%) | 2 (3.5%) | 1 (1.6%) | .6 |
| Unsure | 1 (.8%) | 0 (0%) | 1 (1.6%) | > .9 |
| Tasks integrated into remote work policy [n (%)] | ||||
| Direct patient care (consults, OTVs, follow-up visits) | 69 (57%) | 36 (63%) | 33 (52%) | .2 |
| Clinical documentation | 109 (90%) | 52 (91%) | 57 (89%) | .7 |
| Patient planning (simulation, contouring, plan review/approval) | 105 (87%) | 49 (86%) | 56 (88%) | .8 |
| Patient treatment (IGRT review) | 73 (60%) | 31 (54%) | 42 (66%) | .2 |
| Departmental requirements (chart rounds, education) | 109 (90%) | 51 (89%) | 58 (91%) | .8 |
| Hospital requirements (tumor board, research grand rounds) | 114 (94%) | 54 (95%) | 60 (94%) | > .9 |
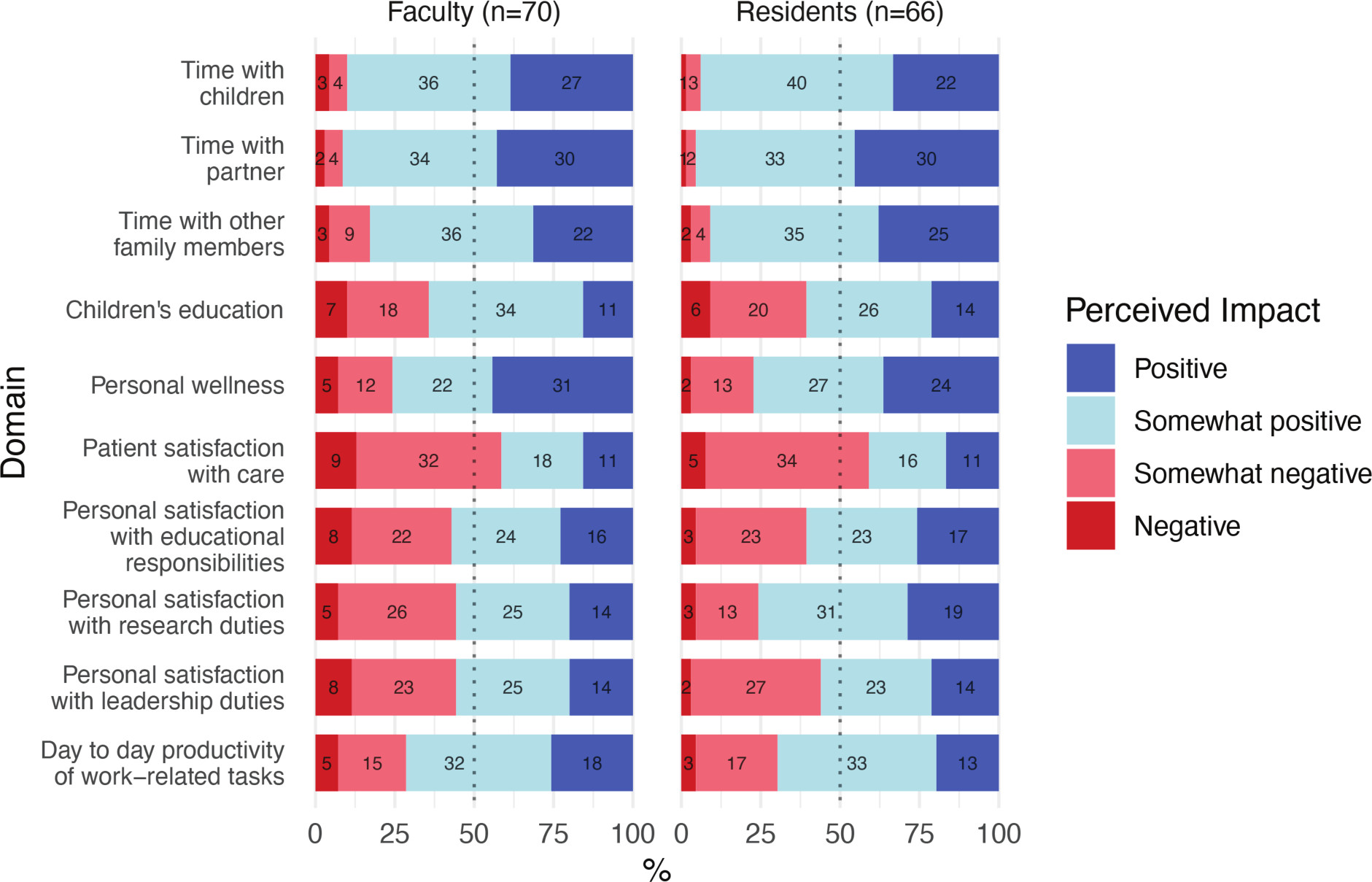
A majority of faculty (> 51%) and residents (> 51%) indicated that WFH was perceived to have a positive or somewhat positive impact on all measured outcomes, except for patient satisfaction with care ( Figure 1 ). Both faculty and residents reported that “time with partner” was the most positively impacted domain, with 91.4% of faculty and 95.4% of residents rating this domain as “positively” or “somewhat positively” impacted by WFH. The only domain in which the degree of satisfaction varied significantly between residents and faculty was research. Nearly half of the faculty (44.3%) indicated that their research duties had either been “somewhat negatively” or “negatively” impacted, while only 19.7% of residents shared this sentiment. Subjective commentary on WFH experiences varied ( Table 3 ).
Perceived impact of work from home on domains of work and life.
Select Participant Quotes Illustrating the Diversity of Views on WFH in RO, Both in Personal and Professional Aspects
| SELECTED RESPONSES FROM PARTICIPANTS REGARDING THEIR PERSONAL EXPERIENCES DURING COVID-19 |
|---|
| “Education and tumor board review via virtual zoom should continue after the pandemic. It is convenient. There is a higher number of participation (easier to sign on than to physically be there). And you can see in detail the radiological image on the shared screen. Plan review with attending and dosimetrists have been very productive virtually (we use Microsoft Teams). Viewing a shared screen is easier than looking over someone else’s shoulder. Remote patient simulation is not possible. You can't learn how to set up a patient without being there in person. Remote OTV is not helpful. I learn better from physically examining the patient. I would prefer consults and follow-ups in person. Many patients have technological issues that degrade the quality of the interaction with the physician. And the inability to perform a physical exam is big problem.” |
| “Work from home is doable for Radiation Oncology faculty for part of the week. 1-2 days of work from home are not disruptive and may improve work-life balance.” |
| “I think working from home has been a positive experience, more time with loved ones at home, more time freed up from less travel to and from work, increased time and energy for patient care, and improved quality of life.” |
| “In the beginning, there was an overreaction with everyone working from home. That was detrimental to spontaneous casual interactions such as conversations between physics, dosimetry and physicians, which are important for improving departmental capabilities over time and continuously educating members of the department (for example, physician teaching a new dosimetrist different ways of planning and physicist debating merits of a certain technique with physician). These productive interactions were greatly missed, but there is an advantage to having at least some time at home with remote meetings and time to catch up and avoid burnout. Plus, it makes [my] spouse happy to have me at home even if I'm in the home office working. I think our department found a balance that works for us, and I assume it will continue in some capacity moving forward.” |
| “Some disease sites are more suited to work from home and some really can't provide good clinical care without in person patient evaluation. If you're a physician treating brain tumors or routine prostate or breast maybe work from home is ok. If you do head and neck or Gyn requiring more invasive or closer examination not amenable to video then you can't provide optimal clinical care on a work from home basis, this disproportionately affects people who are in those specialties.” |
| “It allows me taking care of children education when they are studying from home. I am more efficient using my time without sacrificing patient care. This policy of 1 WFH day will stay in my institution because of good feedback.” |
| “I had a baby in the NICU and the remote work policy allowed me to keep my baby safe while maintaining clinical productivity.” |
| “At times difficult to find quiet spot, but productive. Allowed me to continue breastfeeding longer than I could with my first child since I was home.” |
| “Our therapists and nurses need to be there in person. Physicians and residents should be there managing patients in person with appropriate PPE too. Patient care is optimal in person. I cannot adequately examine a patient through a video screen. One could consider working from home on admin/non-clinical days but that still leaves others to cover clinical work that occurs on those days and that creates additional unnecessary burden on others, esp when working from home may be less productive.” |
Abbreviations : RO, radiation oncology; WFH, working from home.
Discussion
COVID-19 posed significant challenges for RO departments. A total of 87.6% of departments implemented WFH policies in response to the pandemic, reflecting the adaptations that were required to maintain safety and efficiency. This study highlights several aspects of WFH in RO that warrant consideration, including physician satisfaction, burnout, patient care, and gender equity.
Our findings are consistent with current literature relating to RO physician satisfaction during the pandemic, demonstrating that radiation oncologists report decreased burnout with WFH. A survey by Hoffman et al found higher 2020 pre-pandemic burnout rates compared with rates during the pandemic WFH era (40% vs 32%, P < .05, respectively), and most employees (74%) reported having a positive experience with WFH.3 Similarly, we found that RO faculty and residents perceived positive WFH-related impacts. More specifically, 90% of faculty and 93.9% of residents reported a positive or somewhat positive impact on their time with children. Additionally, 75.7% of faculty and 77.3% of residents perceived a somewhat positive or positive impact on their personal wellness. This suggests that WFH may improve the overall quality of life for some RO employees.
Despite the positive impacts of WFH on RO job satisfaction, research suggests that clinical employees are more likely to experience decreased productivity while working from home. A study by Shih et al found that research (63%) and administrative (75%) employees reported stability or an increase in their productivity, whereas clinical staff reported decreased productivity with remote work, an important consideration for evolving policies. More specifically, some limitations of WFH for clinical care include the inability to reliably take vital signs, the inability to quickly handle emergencies, and the potential degradation of the patient-provider relationship.8 While telemedicine has drawbacks, it allows for increased access to health care, as patients do not need to travel to their appointments and can decrease lost wages or other financial burdens of attending physician appointments. Additionally, patients who are immunocompromised, such as cancer patients, can have their appointments without being exposed to other patients who may spread infectious diseases in an office setting.9 Moving forward, technological advancements will likely improve the quality of virtual health care, reduce patient and provider costs, and streamline electronic communication with patients and colleagues, which may mitigate clinical staff concerns.10 There may also be a need for identifying tangible performance objectives that ensure RO employees can thrive in all settings.
Lastly, our study found that departments with a higher percentage of women were more likely to have WFH policies and more flexible options ( Table 2 , comments 6-8). Our results also showed that WFH can improve domestic tasks for women with children, but also highlighted the need for considering the unique challenges faced by female physicians in WFH policy decisions.5 , 6 Policy changes that could help with work-life balance include allowing employees to keep their cameras on or off according to their preferences and needs at work meetings, which could allow for more privacy for employees to complete activities such as breastfeeding while participating in work meetings. In addition to flexible on-screen policies, a culture of acceptance for children or pets in the background of video calls that are not patient-facing can normalize the struggles to find balance for all employed people. Finally, designating virtual days on which employees have all of their virtual appointments on 1 day of the week and allowing for those with academic days to complete them remotely can decrease commute time, allow for more personalization of one’s schedule, and increase efficiency.
Limitations of the study include assessing only academic departments with a limited number of participants and a lack of data on the impact of technology on WFH productivity. Additionally, this survey captures only a specific moment in time and therefore is not entirely reflective of the evolving pandemic-related policy landscape. Further research is needed to improve virtual health care tools and guide policies for clinicians with a balance of tasks that can be completed remotely. These future studies should investigate the effectiveness of hybrid work models, physician satisfaction with these work models, retention of faculty members working with hybrid work models, and patient satisfaction with virtual visits.
Overall, our study highlights the challenges and opportunities presented by WFH in RO during the COVID-19 pandemic. Our findings suggest that more equitable policies may be necessary to support female physicians. Furthermore, this study provides valuable insights that can inform the development of WFH policies that balance the needs of physicians, patients, and the health care system.
To access the complimentary continuing education opportunity associated with this article, please visit Applied Radiation Oncology Continuing Education.
References
Footnotes
Data sharing statement
All data generated and analyzed during this study are included in this published article.
Disclosures
The authors have no conflicts of interest to disclose. None of the authors received outside funding for the production of this original manuscript. Results of this study were presented in the poster session: Dalwadi S. Patterns in attending and resident remote work policies in academic radiation oncology departments. Poster presented at: American Society for Radiation Oncology Annual Meeting; October 24-27, 2021: Chicago, IL. No other part of this article has been previously published elsewhere.
Citation
Ponce SB, LoTemplio A, Kaya E, Lichter K, Dalwadi SM, Sinha S, Wairiri L, Stadtlander W, McGunigal M, Jagsi R, DPhil, Osborn VW, Jeans E, Peters GW, Kahn JM. Adapting to the Virtual World: An Analysis of Remote Work Policies in Academic Radiation Oncology. Appl Radiat Oncol. 2024;(1):6 - 14.
doi:10.37549/ARO-D-24-00003
March 1, 2024