Radiation Therapy for the Management of Refractory Giant Condyloma Acuminata: A Case Report
Affiliations
- 1 Department of Radiation Oncology, University of California San Francisco, San Francisco, CA
- 2 Department of Radiation Oncology, Keck School of Medicine, University of Southern California, Los Angeles, CA
Giant condyloma acuminata (GCA), also known as Buschke-Löwenstein tumor, is a rare human papillomavirus-related lesion that can affect the anorectal region and is characterized by aggressive local growth and a high recurrence rate. This case report details a 46-year-old immunocompetent man with refractory anorectal GCA that recurred despite multiple surgical interventions, including abdominoperineal resection (APR). Due to the extensive and refractory nature of the recurrent disease following APR, definitive radiation therapy was offered. Intensity-modulated radiation therapy to 50 Gy in 25 fractions resulted in rapid disease regression, symptom relief, and a complete clinical and metabolic response. This case highlights the efficacy of radiation therapy in managing challenging GCA cases.
Case Summary
A 43-year-old HIV-negative, immunocompetent man initially presented to the anal neoplasia clinic with a several-month history of growing, friable pink lesions in the anal area. These lesions extended from the perianal skin to the anal verge and were associated with significant anal pain. He underwent local excision and hyfrecation of extensive condylomas. Pathology of 2 excised lesions showed low-grade squamous intraepithelial lesions, positive for low-risk human papillomavirus (HPV) by in situ hybridization. Unfortunately, he developed rapid local recurrence within 1 month of this initial surgery. Despite subsequent repeat excision/fulguration procedures (6 in total) over a 3-year period, followed by an abdominoperineal resection (APR) with rectus myocutaneous flap reconstruction, the condylomas continued to recur aggressively.
Diagnosis
Repeated histopathology of the excised lesions, including the extensively sampled APR specimen, revealed well-differentiated squamous epithelium with orderly maturation, marked acanthosis with hyperkeratosis, associated with low-risk HPV positivity, high-risk HPV negativity, and without any high-grade dysplasia. An institutional next-generation sequencing (NGS) panel identified an activating hotspot mutation in the TERT gene promoter, inactivating frameshifts in KMT2B and KMT2D , and an inactivating nonsense mutation in NOTCH3 . Few large-scale chromosomal alterations were noted, including a gain of distal 7q and loss of interstitial 7q. Overall, the lack of large-scale copy number changes and absence of TP53 or CDKN2A alterations, along with the benign histology with low-risk HPV positivity and high-risk HPV negativity throughout an extensively sampled tumor, were most consistent with giant condyloma acuminatum without clear evidence of malignant transformation.
Imaging Findings
His post-APR course was complicated by wound-healing issues, persistent drainage, and the development of intra-abdominal abscesses and suspected fistulas connecting the bladder, rectal stump, and perineal wound. Recurrent condylomas appeared at the perineal incision site within 6 months, extending to the anterior aspect of the perineum and scrotum. Further surgery was felt not to be feasible, and the patient was referred for multidisciplinary discussion with radiation oncology and medical oncology. An F-18 fluorodeoxyglucose (FDG) PET/CT was obtained, which showed extensive abnormal enhancement and marked hypermetabolism in the pelvis ( Figure 1A ), including abnormal hypermetabolic tissue along multiple fistulous and percutaneous drain tracts. The bladder was abnormally thickened, though a cystoscopy and Foley catheter placement under anesthesia by urology did not identify clear involvement of the bladder. At this time, both definitive chemoradiation or radiation alone were felt to be reasonable options, and the risks and benefits of both were presented to the patient, who expressed a strong desire to avoid chemotherapy. Given the lack of evidence of malignant transformation in his extensively sampled APR specimen, radiation alone was offered.
Pre- and post-radiation F-18 fluorodeoxyglucose (FDG) PET/CT fusion images. Pre-radiation FDG PET/CT (A) showing extensive abnormal hypermetabolism in the pelvis, including extensions anteriorly and posterolaterally along fistulous tracts. Axial, sagittal, and coronal views of radiation treatment plan (B), with high-risk volume (50 Gy) outlined in red and pelvic field (45 Gy) outlined in orange. Pre-radiation attenuation-corrected PET (C) showing disease extending posteriorly and anteriorly as indicated by red arrows. Post-radiation attenuation-corrected PET (D) obtained 7 weeks after treatment showing complete metabolic response.
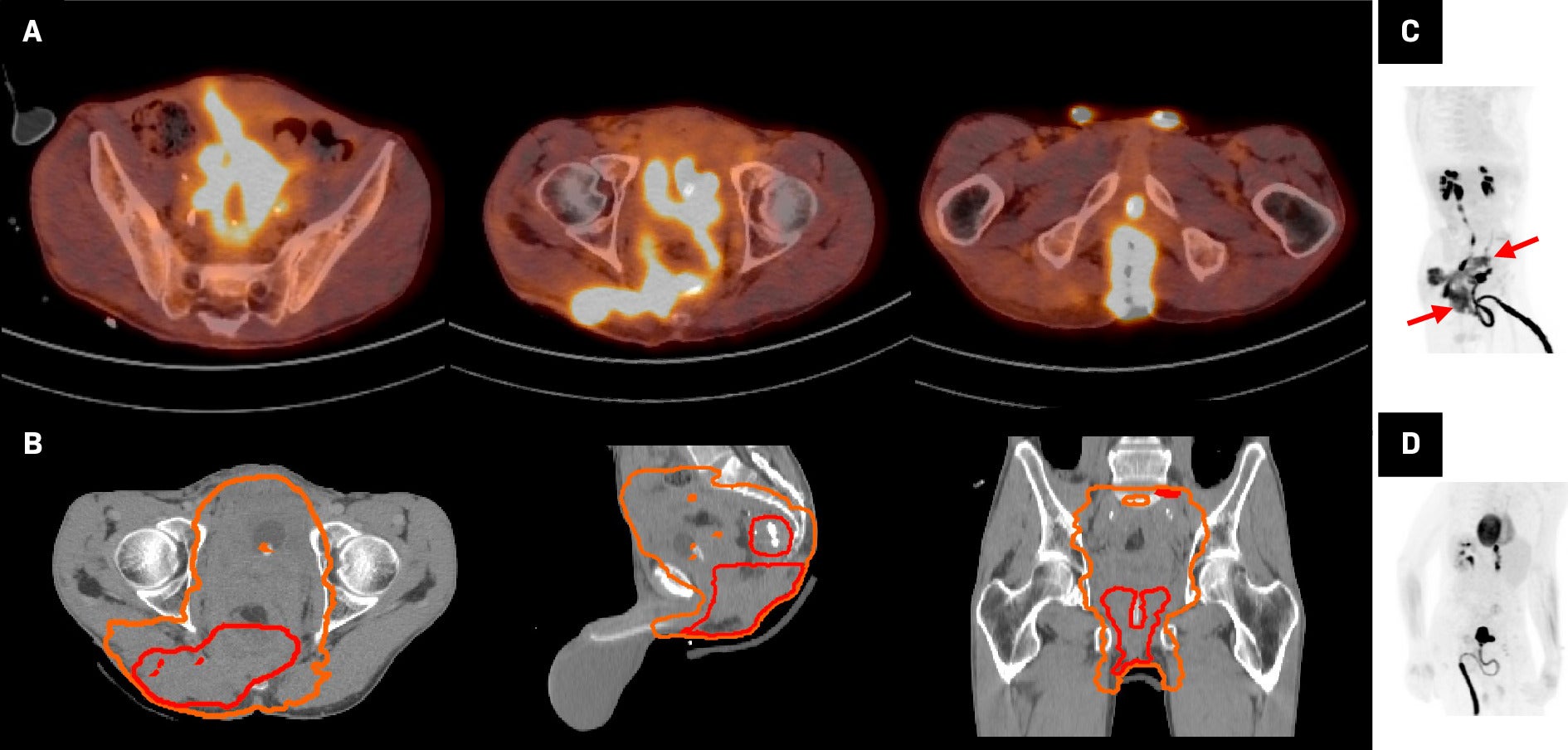
The patient received 50 Gy in 25 fractions to a high-risk volume and 45 Gy in 25 fractions to a larger pelvic field via a volumetric modulated arc therapy plan encompassing all areas of FDG avidity ( Figure 1B ). The high-risk volume receiving 50 Gy was delineated based on FDG PET avid areas and regions of abnormal contrast enhancement on CT. A 2-3 cm customized expansion was used to delineate a clinical target volume (CTV) respecting anatomic boundaries. The CTV was also expanded to include the pelvis, with a superior border of L5/S1, encompassing the entire prior surgical field and all potential fistulous tracts, and received 45 Gy. Treatment was well tolerated with grade 2 radiation dermatitis and mild fatigue. Rapid regression of his condylomas was noted during the treatment course ( Figure 2 ), along with a significant decrease in drain output and an improvement in pain levels. By the end of treatment, the condylomas had completely regressed, leaving behind a large perineal cavity. An FDG PET/CT obtained 7 weeks post-radiation showed a complete metabolic response ( Figure 1C , Figure 1D ). At 7 months post-radiation, he remains recurrence free and is presently undergoing hyperbaric oxygen therapy to assist healing of his fistulas and perineal cavity.
Image series of the patient’s response to treatment. Images taken at various time points, including before beginning treatment, during treatment, and after the completion of treatment.

Discussion
Giant condyloma acuminata (GCA), also known as Buschke-Löwenstein tumor, is a rare and aggressive form of condyloma acuminata, characterized by benign histology, which belies its persistent and locally destructive growth, high risk of recurrence, and potential for malignant transformation.1, 2 Although associated with low-risk HPV (HPV-6 and HPV-11) and characterized by benign histological appearance, GCA can exhibit clinical behavior akin to malignant tumors, including aggressive tissue infiltration and destruction, a high rate of recurrence, and a mortality rate of up to 20%-30% in historical series.3, 4
Genomic characteristics of GCA have rarely been reported, and the biological underpinnings of its pathogenesis are poorly understood.1 Among the alterations found via NGS in this case, KMT2B and KMT2D are mutations that affect histone methyltransferases, which may contribute to epigenetic dysregulation and have been reported in many cancer types, notably in squamous cell carcinomas of the lung, esophagus, anus, and head and neck.5 An activating TERT promoter hotspot mutation was also seen; activating TERT promoter mutations have been identified frequently in many cancer types and in pre-cancerous settings.6 The NGS also revealed few large-scale chromosomal losses or gains, which are much more commonly seen in anal squamous cell carcinomas.7
Traditionally, GCA is managed through locoregional therapies, including topical therapies, wide local excision, or APR. A literature review of 42 cases of surgically managed GCA found that up to 56% of these tumors were associated with histologically confirmed malignancy, underlining the high malignant risk of these tumors.3 Moreover, GCA were frequently associated with deep infiltration of surrounding structures and formation of fistulas filled with condylomas. Our case highlights the utility of FDG PET in delineating the full extent of involvement with GCA as condylomatous involvement of the deep pelvis and fistulous tracts had not been suspected, but was evident on the pre-radiation therapy FDG PET. Indeed, intense FDG avidity within condyloma acuminata has previously been described in case reports, but the use of FDG PET for GCA has not, to our knowledge, been reported on before.8 - 10
Reports of definitive radiation therapy for GCA remain rare, but the existing examples suggest that radiation therapy is a viable treatment option for managing refractory GCA and condyloma acuminata. Moodley and Govender reported on 54 HIV-positive patients with unresectable vulvar GCA treated with 30 Gy in 10 fractions, resulting in a 30% complete response and 61% partial response rate.11 Partial responders received further local therapies, and 52 of 54 (96%) of patients were recurrence free at 5 years. Dhadda et al reported complete regression of extensive genital warts incidentally within a postoperative vulvar radiation field treated with 40 Gy in 15 fractions.12 Sobrado et al reported complete response to 45 Gy in 25 fractions of a large recurrent perianal GCA with fistulous involvement, with the patient remaining disease free through 20 months of follow-up.13 Kim et al describe a case of a giant perianal condyloma recurrent after APR, successfully treated with 45 Gy in 15 fractions with apparent complete clinical response at 6 weeks post-radiation therapy.14 Sivapalan et al reported complete clinical response to 50.4 Gy in 28 fractions of a perianal GCA with deep pelvic infiltration extending into the mesorectal and periprostatic space, with the patient remaining disease free at 6 months of follow-up.15 They also provided a literature review of 8 cases of GCA associated with histologically confirmed malignancy and 3 cases of GCA without histologic confirmation of malignancy, treated with definitive chemoradiation. Of these 11 cases, 3 developed recurrences, an outcome similar to that of anal squamous cell carcinoma. These data and the present case suggest that radiation therapy may be an effective therapy for GCA in cases where traditional treatments are inadequate, providing effective local control and potential disease regression, particularly in cases with clearly benign histology of condyloma acuminata. The effectiveness of radiation therapy in the definitive setting also lends support to its efficacy in the neoadjuvant setting, which may be particularly important in maximizing the opportunities for avoidance of permanent colostomy. Multidisciplinary discussion is essential to improve outcomes of patients with this rare and often complex condition.
Key takeaways from the present case include the utility of FDG PET in delineating the true extent of pelvic involvement of GCA, and the unexpectedly extensive imaging findings identified during workup of this case underlines the potential of GCA to infiltrate insidiously within the pelvis, particularly along surgical and fistulous tracts. Additionally, the GCA in the present case was extensively sampled and examined by pathology over time, including with an NGS panel, without evidence of malignant transformation, which provided equipoise regarding treatment with definitive radiation therapy or chemoradiotherapy and patient-centered decision-making.
Conclusion
This case illustrates the usefulness of radiation therapy in the management of GCA. A multidisciplinary approach is essential for optimizing management strategies and improving patient outcomes in this complex condition.
References
Citation
PG W, S T, WC C. Radiation Therapy for the Management of Refractory Giant Condyloma Acuminata: A Case Report. Appl Radiat Oncol. 2025;(1):42-46.
doi:10.37549/ARO-D-24-00029
March 1, 2025