Added Dimensions: 3-D Printing Applications in Radiation Oncology
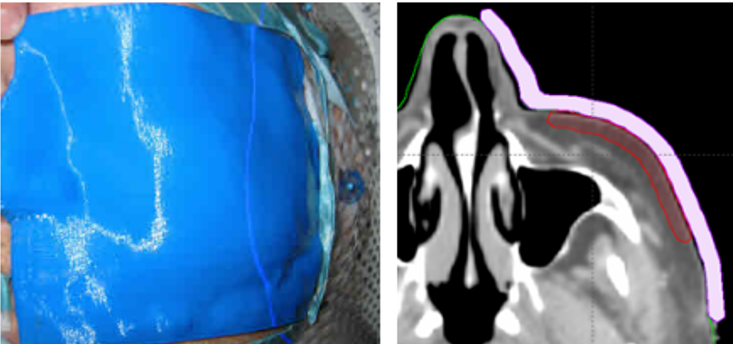
Figure 1. A 3-D printed bolus (left), which uses the nose as an anchor point for set-up accuracy and consistency during radiation therapy. images/courtesy Adaptiiv
Three-dimensional (3-D) printing is a rapidly growing technology in radiation oncology, enabling the creation of custom devices used to treat patients and materials for educational simulation. The layer-by-layer manufacturing process that directly produces an object from 3-D digital data1 has evolved to become a practical, affordable means of optimizing individual treatments, improving workflows, and enhancing patient care through fabrication of high-quality, custom tools and accessories.
As the costs of both printers and materials have receded in recent years, 3-D printing has become a go-to for physicists in radiation oncology departments who are used to “building things to make things happen,” says Jeremy Donaghue, MS, DABR, medical physicist at the Cleveland Clinic Moll Cancer Center at Fairview Hospital.
“In the last couple years, 3-D printers have really started to become more available and usable to the public, which has given us an opportunity to be more exact,” Donaghue says, noting the benefits of affordable pricing, precise customization, and fast turnaround.
“There’s been a shift in 3-D printing in that it’s becoming more ubiquitous in radiation oncology applications,” agrees Steve Braunstein, MD, PhD, associate professor and vice chair of the department of radiation oncology and SRS program co-director at the University of California, San Francisco. “Factors have aligned in terms of affordability, ease and comfort of use, and the ability of users to collaborate with their particular applications. All of this has led to lot of enthusiasm right now.”
While 3-D printing in health care hit the mainstream in specialties such as dentistry and orthopedics years ago, radiation oncology is just beginning to realize its diverse potential of applications to augment clinical precision and access to personalized care, particularly for treatments areas with complex geometries. For functions that traditionally require manual fabrication such as production of phantoms, bolus, and patient-specific brachytherapy applicators, treatment teams are leveraging user-friendly software packages to sculpt features from anatomic imaging for exact and efficient modeling.
A Team Approach
Due to its relative nascence in the specialty, no particular framework exists for determining authority over new applications for 3-D printing, although experts agree that medical physicists will play a primary role.
“As radiation oncologists, we’re tethered to our physicists in this very technical field. Those with a background in medical physics and engineering are generally comfortable in this arena with 3-D fabrication, software development and deployment technologies,” Dr. Braunstein says.
Dan Golden, MD, MHPE, associate professor of radiation and cellular oncology at the University of Chicago, who has been using 3-D printing for 8 years, concurs. “In our clinic, the physicist has the lead on doing the 3-D printing. As a physician, it’s my role to say what we need to treat, and then it’s up to the physicist, therapist, and physician to work together to figure out the best way to treat it.”
“In rad onc, a lot of the implementation is driven by physicists, but at the same time, we’re a team,” Donaghue adds. “Anyone can bring up the idea [of 3-D printing]—the therapist, dosimetrist, or radiation oncologist—and we talk about it. But from my perspective, it’s up to the physicists to figure it out.”
In his role, Donaghue sees 3-D printing as the ideal means to manufacture solutions that will fix or improve setups that make his department better overall. For example, he made a phantom for $20 to test the consistency of a couch with 6 degrees of freedom—“good practice,” he says. “I wasn’t willing to ask my organization to spend a few hundred dollars on something that wasn’t necessarily required when I can develop it myself. I could take control and drop the cost,” Donaghue explains, adding he also 3-D printed a wall-mounted box for a piece of electronics used on a daily QA device that hung by its cables and repeatedly fell.
“Three-D printing gives us the ability to simply make things,” he says, “which can make the department better.”
Customizing Radiation Treatment
Three-D printing applications go well beyond departmental patches, and are most commonly utilized in radiation treatment customization for procedure devices such as bolus in radiation therapy and brachytherapy applicators. For instance, 3-D printed, patient-specific bolus offers a more precise patient fit and optimized dose distribution for hard-to-treat areas of the skin, including head and neck targets (see Figure 1). Traditional manually fabricated bolus is made of a rubber-like material draped as a sheet, which often fails to adhere to irregular surfaces, explains Dr. Golden, who initially printed bolus for postmastectomy patients when he realized it was useful for hard-to-treat locations like the nose, under the eye, or behind the ear.
“In my clinic, 99% of 3-D printed applications is for bolus. It’s a very nice tool to have from a clinical standpoint for treating skin cancer in some of these unusual treatment locations,” Dr. Golden says. “We have gotten really good at doing 3-D printing for these areas. We take a scan of the area we want to treat. One of our physicists creates the bolus in the computer system…and she prints a mold, pouring silicone into it,” which solidifies for use, he explains, adding that the silicone makes for a more comfortable patient experience.
Dr. Golden’s clinic uses Adaptiiv Medical Technologies’ FDA 510(k)-cleared software platform to design and create the 3-D printed boluses.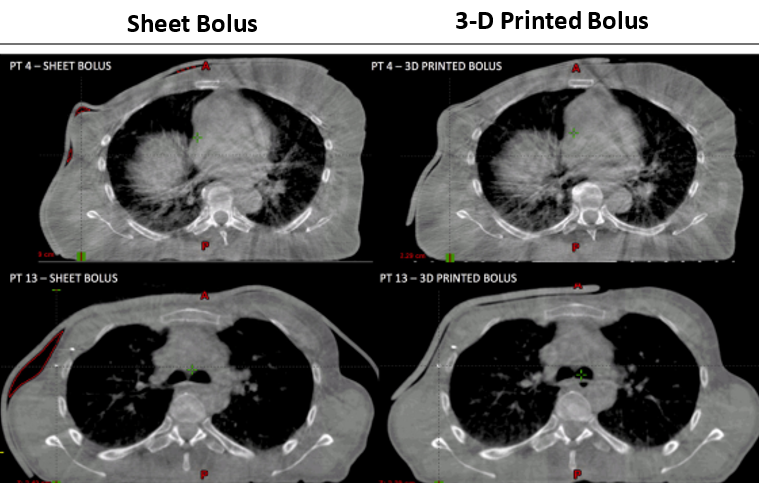
Figure 2. The frequency of air gaps 5 mm or greater can be reduced from 30% to 13% when using 3-D printed bolus.2
“A precise, accurate fit of the bolus is important to reduce inadvertent air gaps between the bolus and the skin, which can result in a lesser dose to affected areas,”2 (see Figure 2) says James Robar, PhD, FCCPM, professor of radiation oncology at Dalhousie University, chief of medical physics at Nova Scotia Health, and co-founder at Adaptiiv.
For example, at the basal cell layer for a 6-MV photon beam, underdosing can occur by up to 4% and 10% for 4 mm and 10 mm air gaps below the bolus, respectively, depending on field size and angle of incidence,3 Dr. Robar explains noting that Adaptiiv’s solution can reduce maximum air gap dimension by up to 40%.2
“Using 3-D-printed bolus provides better fit, superior spatial fidelity, and consistency for each treatment fraction,” Dr. Robar says, adding “most importantly, patient comfort and overall experience is improved.”
Donaghue explains that traditional boluses made from thermoplastic material tend to shrink overtime, which often forces the therapist to apply pressure during positioning. “When the material shrinks, it may pull off your target, and you want to have good contact,” he says. “The skin or scalp tends to be inflamed and painful, so you really don’t want to be pushing down on it. We have less shrinkage generating these 3-D boluses.”
The materials used in custom 3-D printing are approved from a regulatory standpoint as appropriate for medical intervention, Dr. Braunstein notes, also citing improved comfort and durability.
“This ability to 3-D print gave us a lot more control, to really be attuned to the nuances of the anatomy. Using 3-D volumetric imaging to help fabricate the silicone is a very easy transition to 3-D applications in custom bolus as well as brachytherapy.”
The ability to design and print custom brachytherapy applicators for patients using 3-D printing and advanced imaging in the planning process has been significant. After scanning the patient, the treatment team identifies the target area and creates a mold with channels for the radioactive materials that the software has defined, which gets hooked up to the after-loader, Dr. Golden summarizes.
The applicators are ideal for treating areas such as the oral cavity or genitourinary system, says Dr. Braunstein, who prints at UCSF with an industrial, small-scale 3-D printer. “When we’re inserting radioactive materials through a catheter, custom-fabricated applicators more tightly conform to the anatomic space and allow delivery of better, more geometrically precise radiotherapy.”
Educational Simulation
In addition to customization of patient treatment, 3-D printing is proving useful in hands-on education of medical students and resident physicians. As a resident, Dr. Golden recalls his training included an orange taped to the table, simulating the prostate.
“Thanks to 3-D printing, today we’re able to simulate with a 3-D-printed phantom where the bladder and rectum are on ultrasound—a whole other level of simulation—something an orange can’t replicate,” he says.
Three-D printed models simulate high-stakes, real-world procedures that residents otherwise may not get the opportunity to perform hands-on. These models are a low-cost solution for disseminating educational simulation techniques across institutions.
“Rad onc as a specialty has a strong procedural component, especially around brachytherapy, for example,” says Dr. Braunstein. “The actual implantation of radiation sources has a challenging learning curve, and it is very operator dependent. With sophisticated 3-D printing applications, we’re now able to replicate tissue with models that have the same imaging characteristics that real tissue would have under ultrasound, which is very important for proper education and simulation.”
Going to Print: A Promising Future
As radiation oncology applications in 3-D printing continue to advance, physicists and radiation oncologists can learn valuable lessons from those who have successfully deployed solutions, says Dr. Braunstein, both from emergent literature and presentations at annual meetings. Current 3-D applications could “shake up the industry quite a bit,” he adds, noting the expanding potential of certain 3-D printed accessories to replace manufacturer-supplied products due to facilitation by simple, user-friendly software.
“Precision and accuracy are critical to our field, and 3-D printing will lead us toward greater precision, accuracy, and speed in our clinical work, research, and training,” says Dr. Braunstein.
References
- Asfia A, Novak J, Mohammed M, Rolfe B, Kron T. A review of 3D printed patient specific immobilisation devices in radiotherapy. Phys Imag Radiat Oncol, 2020;(13):30-35. Accessed March 2023. https://doi.org/10.1016/j.phro.2020.03.003
- Robar J, Moran K, Allan J, et al. 2017. Intrapatient study comparing 3D printed bolus versus standard vinyl gel sheet bolus for postmastectomy chest wall radiation therapy. Pract Radiat Oncol. 8(4), 221-229.
- Butson MJ, Cheung T, Yu P, et al. Effects on skin dose from unwanted air gaps under bolus in photon beam radiotherapy. Radiat Meas. 2000;32:201-204.