Wernicke’s Encephalopathy Secondary to Severe Malnutrition After Definitive Chemoradiation for Oropharyngeal Squamous Cell Carci
Images



CASE SUMMARY
A 59-year-old female former smoker, never-drinker, diagnosed with cT1N1 p16+ squamous cell carcinoma of the right tonsil (stage I) received definitive chemoradiation at a community cancer center. Her treatment course was complicated by dehydration, weight loss (28%), dysphagia, oral mucositis and candidiasis. The patient was not evaluated by a dietitian, and neither received nutrition supplements nor was recommended for a percutaneous endoscopic gastrostomy (PEG) tube during her treatment course. She completed a total dose of 66 Gy in 33 fractions to the right tonsil/ipsilateral involved neck utilizing an intensity-modulated radiation therapy (IMRT) step-blocking technique with concurrent platinum-based chemotherapy. Six weeks after treatment, she presented to a local emergency department with altered mental status, lethargy and failure to thrive. Due to lack of symptom improvement, she transferred her care to our institution. Physical examination was consistent with acute encephalopathy, nystagmus, diplopia, asterixis, ataxia and clonus.
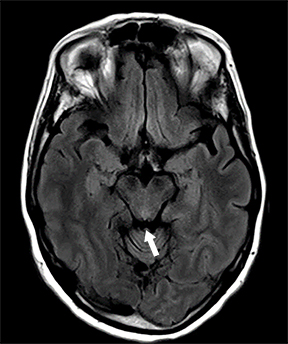
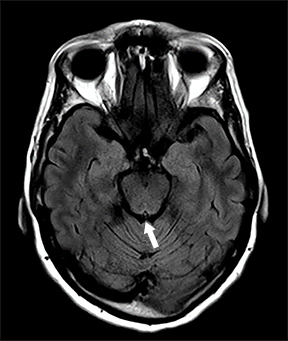
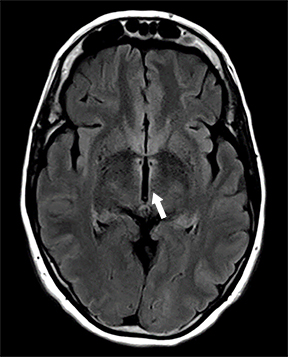
IMAGE FINDINGS
Brain MRI fluid-attenuated inversion recovery (FLAIR) sequence showed hyperintensity of the hypothalamus, margins of the third ventricle, and tectal plate (Figures 1 A-C). Other findings included enhancement of the inferior tectal plate involving the inferior colliculus. Follow-up MRI 1 year later showed resolution of previous findings (Figures 1 D-F).
DIAGNOSIS
The patient presented with a painless enlarged right level II mass. Excisional biopsy of the lymph node was positive for metastatic poorly differentiated squamous cell carcinoma p16+. Right tonsil biopsy demonstrated p16+ nonkeratinizing squamous cell carcinoma. A staging pretreatment positron emission tomography/computed tomography (PET/CT) scan was obtained.
The workup to evaluate the etiology for encephalopathy included brain MRI; lumbar puncture with cell count, protein, cytology, autoimmune/paraneoplastic/encephalitis panel; GQ1b antibodies; HIV test; thiamine and B12 levels. Thiamine levels were noted to be significantly low. The rest of her workup was negative. She was started empirically on IV antibiotics and high-dose thiamine. Her neurologic symptoms started to improve the following day and the patient was diagnosed with nonalcoholic Wernicke’s encephalopathy (WE). Of note, the patient did not have a known genetic or underlying predisposition to develop this condition.
DISCUSSION
The triad of altered mental status, ophthalmoplegia, and ataxia was described by Carl Wernicke in 1881, and in the 1930s thiamine (vitamin B1) deficiency in the context of alcoholism was ascribed to be the culprit. Since then, we have come to learn and understand that malnourishment in the setting of alcoholism is not the only cause of WE. Any condition that leads to severe malnourishment/vitamin B1 deficiency, such as infection, chronic diseases, and cancer can cause WE. Patients with cancer of the head and neck are especially vulnerable to malnutrition due to treatment side effects, such as mucositis, dysphagia, poor oral intake, and weight loss.
Case reports of WE in nonalcoholic patients with cancer of the head and neck are rare, with only a few cases reported in the literature.1,2 In a Lancet systematic review of 129 cases of cancer patients with WE, only one-third of patients presented with the classic triad of symptoms, and only 7 cases (5%) were head and neck cancers. Twenty-eight patients received radiation therapy as part of their treatment, and only 6 (21%) of the patients who developed WE in this group received head and neck radiation, with a median time of 3 weeks since their last fraction.3 Our patient started to exhibit her first neurologic symptoms approximately 6 weeks after treatment completion.
Clinicians often have difficulties and delays in diagnosing cancer-related WE, possibly due to variability in clinical presentation, different diagnostic criteria, and lack of clinical suspicion, with up to 17% of patients diagnosed postmortem in a case series study.3 Prompt recognition of the entity and early treatment are key, since only about a third of the patients will be able to achieve a complete full clinical recovery.3 Therefore, empiric treatment with high doses of thiamine are recommended when clinical suspicion is high. One year after diagnosis and treatment, our patient has not fully recovered from her neurologic symptoms, with persistent ataxia and memory impairment despite having normal thiamine levels and an unremarkable brain MRI. Currently, she has no evidence of disease from her primary head and neck malignancy.
It is important to recognize that head and neck cancer treatment-related toxicities could lead to poor oral intake, dehydration, weight loss, malnutrition and a negative impact on the outcomes and quality of life of these patients.4 For example, different series of patients treated for locally advanced head and neck cancer have reported rates of PEG tube placement as high as 50% to 70%.5 Therefore, preventive measurements, close monitoring and early symptom management such as the use of serial intravenous hydration, implementation of a feeding tube, and professional nutritional counseling are recommended and required during treatment.6
Also well known is the importance of multidisciplinary care in head and neck cancer patients.7 Furthermore, it has been reported that these patients when treated at high-volume radiation centers (ie, those that treat the top one-third of their region’s total patient volume), centers with high clinical trial accrual (≥ 42 patients per center), and by high-volume head and neck radiation oncologists will have better oncologic outcomes and lower treatment-related toxicities.8-10
CONCLUSIONS
Nonalcoholic WE or thiamine-related encephalopathy is an acute neurologic complication. Cancer patients, particularly those with head and neck cancers who have completed definitive chemoradiation, can be at risk due to severe malnutrition associated with acute treatment-related toxicities. It is important that oncologists are familiar with the potential causes, symptoms, diagnostic criteria and management of this serious condition. This case underscores the critical role of multidisciplinary care at a high-volume institution in managing head and neck cancer patients.
REFERENCES
- Kawabe M, Noguchi K, Kishimoto H, et al. Wernicke’s encephalopathy after chemoradiotherapy for tongue cancer: report of a case. Oral Sci Int. 2013;10(2):100-101.
- Fikhman G, Berger JR, Gal TJ. Wernicke’s encephalopathy in the course of chemoradiotherapy for head and neck cancer. Am J Otolaryngol. 2011;32:250-252.
- Isenberg-Grzeda E, Rahane S, Derosa AP, et al. Wernicke-Korsakoff syndrome in patients with cancer: a systematic review. Lancet Oncol. 2016;17:e142-148.
- Van den Berg MA, Rasmussen-Conrad EL, Van Nispen L, et al. A prospective study on malnutrition and quality of life in patients with head and neck cancer. Oral Oncol. 2008;44:830-837.
- Koyfman SA, Adelstein DJ. Enteral feeding tubes in patients undergoing definitive chemoradiation therapy for head-and-neck cancer: a critical review. Int J Radiation Oncol Biol Phys. 2012;84(3):581-589.
- Paccagnella A, Morello M, Da Mosto MC, et al. Early nutritional intervention improves treatment tolerance and outcomes in head and neck cancer patients undergoing concurrent chemoradiotherapy. Support Care Cancer. 2010;18:837-845.
- Light T, El Rassi E, Maggiore RJ, et al. Improving outcomes in veterans with oropharyngeal squamous cell carcinoma through implementation of a multidisciplinary clinic. Head Neck. 2017;39:1106-1112.
- Naghavi AO, Echevarria MI, Strom TJ, et al. Patient choice for high-volume center radiation impacts head and neck cancer outcome. Cancer Med. 2018;7:4964-4979.
- Wuthrick EJ, Zhang Q, Machtay M, et al. Institutional clinical trial accrual volume and survival of patients with head and neck cancer. J Clin Oncol. 2015;33(2):156-164.
- Boero IJ, Paravati AJ, Xu B, et al. Importance of radiation oncologist experience among patients with head and neck cancer treated with intensity-modulated radiation therapy. J Clin Oncol. 2016;34:684-690.
Citation
MN B, D M, DM B, S B, S J, ME G. Wernicke’s Encephalopathy Secondary to Severe Malnutrition After Definitive Chemoradiation for Oropharyngeal Squamous Cell Carci. Appl Radiat Oncol. 2020;(3):33-35.
September 9, 2020