Severe contact dermatitis secondary to metal contaminants in radiation therapy paint pens
Images


CASE SUMMARY
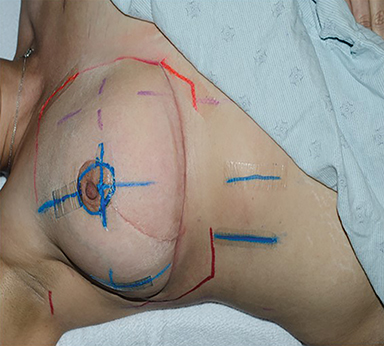
A 31-year-old woman with a cT1cN0M0 ER-positive, PR-negative, HER-2/neu 1+, grade 3 invasive ductal carcinoma underwent segmental mastectomy, breast reduction and sentinel lymph node biopsy confirming pT1cN0 disease with negative margins. Adjuvant chemotherapy was recommended and she received paclitaxel for 12 cycles and fluorouracil for 4 cycles. Subsequently, she underwent treatment planning for whole-breast radiation therapy, 50 Gy in 25 fractions followed by a 10 Gy boost. Standard setup marks were drawn at simulation using the normal order paint pens (Sharpie Paint, medium point, oil-based, Vietnam), (Figure 1A). After 4 weeks of radiation therapy, she developed well-demarcated linear eczematous weeping and erythematous plaques circumferentially around the areola and in linear lines radiating from the right areola corresponding to the paint location (Figure 1B). Upon review, it was established that 4 similar cases had occurred in the previous 8 weeks, whereas none had been observed prior to these.
DIAGNOSIS
The differential diagnosis included infection, allergic contact dermatitis, or radiation interaction with the paint material. Cases were not confined to a single treatment machine. Infection control was contacted and all pens used for patients were collected and cultured. Cultures were negative. Skin cultures from patients demonstrated normal flora. Referral to dermatology suggested contact dermatitis. All patients were determined to likely have been marked with pens from a single lot. The manufacturer stated there had been no change in materials used in manufacture, noting that the dyes are purchased from external distributors and they could not obtain information on dye lots for specific purchases.
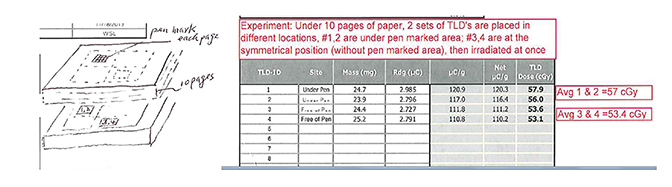
Recognizing that metal is common in tattoo ink, MRI safety screening includes asking about the presence of tattoos. In turn, we hypothesized that metal in the paint pens could lead to contact dermatitis or increased radiation dose received. To test the latter, we applied paint to 10 sheets of paper stacked on top of each other and compared dose through this to a control of unmarked paper using thermoluminescent dosimeters (TLDs). The results interestingly showed that the dose was 7% higher under pen-marked areas, suggesting the pens contribute to a build-up effect or that there is higher Z material in the paint, increasing the dose (Figure 2). We considered that this dose difference would also cause the clinical symptoms noted. Also of note, the patient reported to dermatology that she removed a necklace she had worn for years because it was irritating her skin. The patient was treated with topical steroids, and her symptoms improved. We concluded that a metal contaminant in the paint led to contact dermatitis.
DISCUSSION
Radiation-induced skin reactions or radiation dermatitis are one of the most reported side effects of radiation therapy in cancer patients. These cutaneous reactions can be divided into the categories of acute, consequential late, and chronic.1 Cutaneous reactions can vary from erythema to desquamation to ulceration. Sensitivity to radiation differs in different areas of the body. The most sensitive areas are the anterior neck, chest, extremities, chest, abdomen, face, breast and hair follicles of the scalp.2 Approximately 10% of patients will experience moist desquamation and ulceration, which may result in treatment delays,3 decreased quality of life, and pain.4,5 In light of this, we should be on alert for any other contributing factors that can aggravate these reactions.
In our reported case, we noted skin symptoms inconsistent with expected radiation dermatitis and found that pens used for setup marks caused an allergic reaction. However, the dosimetric findings of a 7% increase in dose makes the possibility that the contact dermatitis and the increased skin reaction from the metallic contaminants may have combined effects. This could be checked by marking the same patient within and outside the radiation field. Different metals such as mercury, cadmium, nickel, cobalt, copper, iron and chromium are used in manufacturing variant colors of tattoo pigments, and these metals can cause allergic reactions in some people. Red pigment commonly causes more allergic reactions than other pigments,6 as it is often made with mercury, to which an estimated 1% to 5% of the general population is allergic.
Additionally, nickel is one of the most common causes of allergic contact dermatitis.7 Unilateral nickel-induced facial dermatitis elicited by cell phone use has been reported.8 Likewise, hairdressers have been diagnosed with allergy-related hand eczema from prolonged skin contact with nickel-containing scissors and crochet hooks.9 Other common causes of contact dermatitis are poison ivy, fragrances and neomycin.7
Contact dermatitis is divided into two categories: irritant contact dermatitis, which is caused by direct cutaneous inflammation or direct skin injury from an irritant; and allergic contact dermatitis, which is caused by type 4 (delayed) hypersensitivity reaction. Allergic contact dermatitis develops after repeated or prolonged exposure to an antigen. When a foreign allergic antigen comes into contact with the skin, it links to skin protein, forming an antigen complex and then activating T cells, leading to sensitization. Upon re-exposure of the skin to the antigen, the activated T cells initiate an inflammatory process, leading to a manifestation associated with contact dermatitis.10 Contact dermatitis usually manifests with pruritus, erythema, pain, vesicles and bullae with relatively well-demarcated borders.10 Diagnosis of contact dermatitis is essentially made by patient history, examination and improvement upon avoidance of the allergic substance. If patient symptoms don’t improve by avoidance and empiric treatment, or the allergen isn’t known, then a patch test may be indicated. All of our patient’s symptoms improved after replacing the pen markers and using topical steroids.
Regarding process improvement, all pens were replaced with the Sharpie Permanent Marker, Fine Point, (Atlanta, Georgia), and a new policy required new pens for each patient. One further incident was identified over a year later in a patient simulated in the main hospital for palliation. It was determined that the simulator in this building had not disposed of all prior pens, leading to this additional case (Figure 3).
CONCLUSION
Paint pens are routinely used in radiation therapy practices for daily setup. These can promote contact dermatitis, and care should be taken to avoid metallic paint pens.
REFERENCES
- Hymes SR, Strom EA, Fife C. Radiation dermatitis: clinical presentation, pathophysiology, and treatment 2006. J Am Acad Dermatol. 2006;54(1):28-46.
- Brown KR, Rzucidlo E. Acute and chronic radiation injury. J Vasc Surg. 2011;53(1 Suppl):15s-21s.
- Isomura M, Oya N, Tachiiri S, et al. IL12RB2 and ABCA1 genes are associated with susceptibility to radiation dermatitis. Clin Cancer Res. 2008;14(20):6683-6689.
- Duncan W, MacDougall RH, Kerr GR, Downing D. Adverse effect of treatment gaps in the outcome of radiotherapy for laryngeal cancer. Radiother Oncol. 1996;41(3):203-207.
- MacDougall RH, Robertson C, Robertson AG, et al. Similar decreases in local tumour control are calculated for treatment protraction and for interruptions in the radiotherapy of carcinoma of the larynx in four centres. Int J Radiat Oncol Biol Phys. 1998 Jan 15;40:319-329.
- Serup J, Sepehri M, Hutton Carlsen K. Classification of tattoo complications in a hospital material of 493 adverse events. Dermatology. 2016;232(6):668-678.
- Fonacier L, Bernstein DI, Pacheco K, et al. Contact dermatitis: a practice parameter-update 2015. J Allergy Clin Immunol Pract. 2015;3(3 Suppl):S1-39.
- Moennich JN, Zirwas M, Jacob SE. Nickel-induced facial dermatitis: adolescents beware of the cell phone. Cutis. 2009;84(4):199-200.
- Thyssen JP, Milting K, Bregnhoj A, et al. Nickel allergy in patch-tested female hairdressers and assessment of nickel release from hairdressers’ scissors and crochet hooks. Contact Dermatitis. 2009;61(5):281-286.
- Usatine RP, Smith MA, Chumley HS, Mayeaux EJ. Chapter 146. Contact Dermatitis. The Color Atlas of Family Medicine, 2e. New York, NY: The McGraw-Hill Companies; 2013.
Citation
I Y, TL S, WA W. Severe contact dermatitis secondary to metal contaminants in radiation therapy paint pens. Appl Radiat Oncol. 2018;(No 4):44-46.
December 20, 2018