Navigating Radiation Oncology Emergencies: Are We Maximizing Inpatient Call for Residents?
Images
Oncological emergencies are defined as “conditions arising from a reversible threat to an organ function, requiring treatment within hours of diagnosis.”1 For inpatient radiation, common emergency indications include spinal cord compression, superior vena cava syndrome, and vaginal bleeding.2 As cancer therapies improve and more people live with metastatic disease, demand for inpatient radiation will likely increase. This raises 2 important questions:
- What is the optimal format for an inpatient call system?
- How can resident education be maximized during inpatient call?
The format for inpatient call varies based on department size and inpatient volume. In an attending-led format, the attending is notified of the consult and is expected to evaluate/treat as needed, only involving the resident as they see fit. In a resident-led format, the resident is expected to independently evaluate the patient and discuss the management plan with the attending. The attending may be a subspecialist (thoracic, central nervous system, etc.), a designated on-call attending from an inpatient service, or an attending on a daily/weekly schedule with clinic duties. Depending on format, resident responsibilities may extend from care coordination to treatment consent and contouring.
In our program, the on-call residents are primarily responsible for seeing all inpatient consults and after-hour patient calls for 1 week. This includes communicating with the primary teams, obtaining patient consents, and contouring treatment volumes. We also recently transitioned to a system in which the on-call resident has no primary service-related clinical responsibilities during this week, although the attendings with whom they staff cases continue to remain in clinic.
The tasks associated with inpatient call vary across institutions. These opportunities can be highly educational as residents learn about radiation toxicities, logistics of urgent radiation therapy, and workup of new cancer diagnoses. The educational value of inpatient call depends on the inpatient volume and the amount of added administrative work (consents, coordination emails, etc.). However, the educational value decreases if consults per week increase or administrative burden is high.
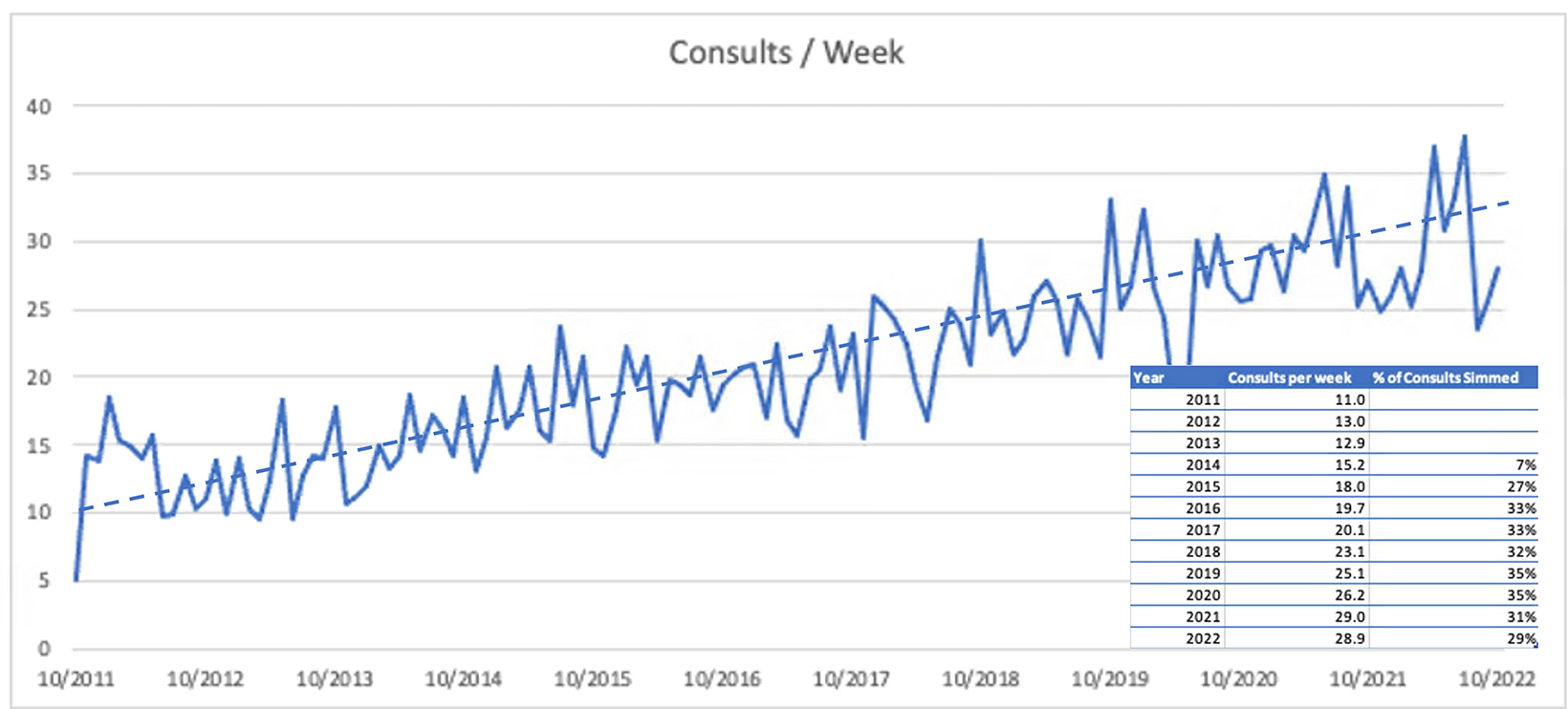
At our hospital, call volumes have risen more than 50% over the last 5 years (Figure 1), with highs approaching more than 40 consults per week in 2022. As the demand for inpatient radiation therapy grows, so will its place in residency training experience. Per the Accreditation Council for Graduate Medical Education (ACGME), duration of on-call weeks is not a prerequisite to meet graduate medical education (GME) requirements in radiation oncology. Although on-call hours are counted toward the 80-hour weekly limit, on-call experiences do not necessarily count toward the 36-month minimum clinical radiation oncology experience, as they are not considered “comprehensive management of patients in treatment.”3 Hence, important considerations are how much the residents should remain involved in inpatient care and whether additional training/lectures are warranted.
Our call system has several advantages overall. As a resident, we gain independence in the patient management thought process. Increased exposure to various palliative scenarios and extensive repetition within those domains boost our confidence in independently evaluating patients, as noted by recent graduates. We also learn to deal with several nuances, especially in a resource-limited setting.
Take-Home Points
A one-size-fits-all approach to inpatient call is not likely, and radiation oncology programs should regularly evaluate their inpatient format to ensure the hospital’s inpatient radiation requirements maximize a resident’s educational experience. In a high-volume center, adjustments may be needed, including excusing residents from normal clinical duties, creating inpatient-specific didactics, forming an inpatient radiation oncology service, or integrating midlevel providers. A nuanced solution to enhance learning and take the experience to the next level may be having PGY5s complete more low-risk palliative cases independently from contours through plan review, all the way to alignment at the machines, with only minimal guidance from attendings. We encourage residency programs to experiment with and share ideas for successful call systems. In doing so, we will be better prepared to expand inpatient radiation services to maximize resident education and effective patient care.
References
- Donato V, Bonfili P, Bulzonetti N, et al. Radiation therapy for oncological emergencies. Anticancer Res. 2001;21(3C):2219-2224.
- Narang M, Mohindra P, Mishra M, Regine W, Kwok Y. Radiation oncology emergencies. Hematol Oncol Clin North Am. 2020;34(1):279-292. doi:10.1016/j. hoc.2019.09.004
- Radiation Oncology Program Requirements and FAQs. Accessed January 19, 2023. https://www.acgme.org/specialties/radiation-oncology/program-requirements-and-faqs-and- applications/
Citation
R U, BD F. Navigating Radiation Oncology Emergencies: Are We Maximizing Inpatient Call for Residents?. Appl Radiat Oncol. 2023;(1):42-43.
March 21, 2023