Gemcitabine-induced radiation recall phenomenon demonstrated by thermography
Images




CASE SUMMARY
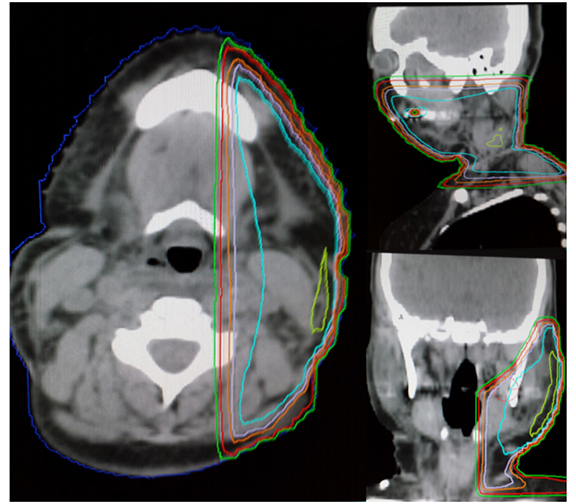
A 51-year-old female was diagnosed with metastatic adenocarcinoma of the lung. She was found to have brain metastases and was treated with whole-brain irradiation to a total dose of 30 Gy in 10 fractions. The patient continued on systemic therapy and was found to have significant tumor burden in the left neck and received palliative radiation to the left upper cervical neck and submandibular area toa total dose of 30 Gy in 10 fractions (Figure 1). She eventually received single-agent gemcitabine (800 mg/m2), and after 2 days she was admitted to the hospital for respiratory failure secondary to facial and neck angioedema. She was found to have normal C4, tryptase, and C1 estersase inhibitor. A thermogram was taken to assist with the diagnosis. She was eventually seen by an oncologist after her airway was stabilized and diagnosed with gemcitabine induced radiation recall.
IMAGING FINDINGS
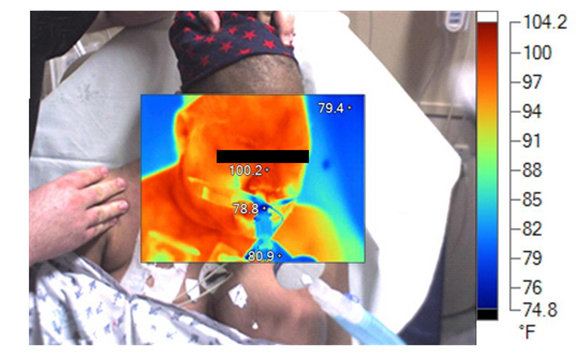
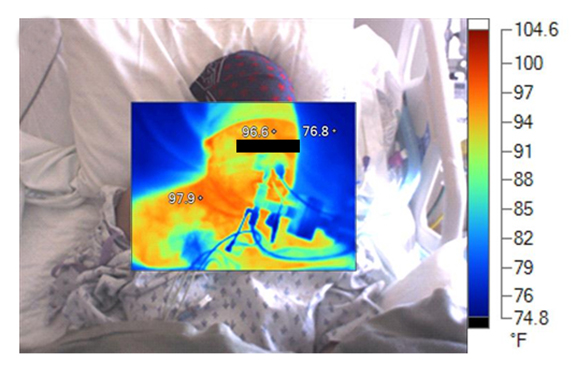
A computed tomography (CT) scan of the neck on 3 days prior to gemicitabine administration shows no evidence of subcutaneous or laryngeal edema. Three weeks later, a CT scan of the neck found diffuse subcutaneous edema with associated laryngeal edema (Figure2). Thermography, on the day of admission, shows a symmetric hyperthermic response with temperatures up to 100.2°F that subsided 2days later (Figure 3).
DIAGNOSIS
Gemcitabine-induced radiation recall with a differential diagnosis of drug reaction, lymphedema secondary to tumor burden, and SVC syndrome.
DISCUSSION
Radiation recall is a phenomenon thought to be related to an inflammatory reaction in a previously irradiated area.1 It was first recognized in the 1950’s after the administration of actinomycin-D.2 It is most recognized in conjunction with older chemotherapeutic agents, such as Adriamycin and even hormonal therapies, such as tamoxifen.3,4 Gemcitabine-induced recall is rare and can easily be missed in the differential diagnosis of clinicians. A series of 6 patients was reported from the Dana-Farber institution that found gemcitabine-induced recall in the central nervous system, skin, gastrointestinal tract, and in the lymphatic and musculoskeletal systems. Our patient presented with diffuse angioedema of the face and neck, after approximately one year from her whole-brain radiation therapy and 4 months from irradiation to the left neck and mandibular area. Thermography has been used to assess radiation injury5 and in a case of a fluoroscopic burn,6 but this is the first known case where thermography was used in the setting of radiation recall. There was an initial hyperthermic reaction that subsided after 2 days, which is in contradistinction to a typical allergic reaction. In the case of idiopathic angioedema, a case report from Japan showed that thermography decreased heat emission in the area of edema, whereas our patient showed homogeneous hyperthermia.7 There is a case of angioedema secondary to gemcitabine reported in 2010; however, in this case the reaction was only 7 minutes after the infusion and angioedema limited just to the right eyelid.8 In addition, the patient had a complete work up with multiple specialists, including allergy, pulmonology, and anesthesia, and none of the typically elevated lab levels were associated with our patient, so the likelihood of this representing an allergic reaction is low. Furthermore, radiation recall presents with dermatitis 63% of the time, while gemcitabine-related events preferentially involve internal tissues and organs.9
CONCLUSION
Radiation recall is a rare event and is believed to be related to an inflammatory reaction in a previously irradiated field after the administration of systemic therapy. Thermography may prove to be a useful tool, especially in the setting of gemicitabine-induced radiation recall with angioedema, where an initial hyperthermic reaction is followed by a decrease in temperature in 2 days. This may be another diagnostic tool to help physicians diagnose this disease. REFERENCES
- Camidge R, Price A. Characterizing the phenomenon of radiation recall dermatitis. Radiother Oncol. 2001;59:237-245.
- D’Angio GJ, Farber S, Maddock CL. Potentiation of x-ray effects by actinomycin D. Radiology. 1959;73:175-177.
- Jeter MD, Janne PA, Brooks S, et al. Gemcitabine-induced radiation recall. Int J Radiat Oncol Biol Phys. 2002;53:394-400.
- Parry BR. Radiation recall induced by tamoxifen. Lancet. 1992;340:49.
- IAEA. Diagnosis and treatment of radiation injuries. Safety Reports Series No 2 1998.
- Goans R, Christensen D. Evaluation of local radiation injury - Part II thermography for fluoroscopy injuries. Health Physics News. 2009.
- Ogasawara T, Kitagawa Y, Ogawa T, et al. MR imaging and thermography of facial angioedema: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:473-476.
- Saif MW, Chakerian P, Kaley K, Lamb L. First case report associating gemcitabine with hypersensitivity reaction in a patient with pancreatic cancer. JOP. 2010;11:273-274.
- Friedlander PA, Bansal R, Schwartz L, et al. Gemcitabine-related radiation recall preferentially involves internal tissue and organs. Cancer. 2004;100:1793-1799.