From Bullet to Canon? Exploring the Promise of Heavy Particle Ion Therapy
Images

Cancer deaths continue to decrease due to advancements in screening, early diagnosis and treatment. According to the American Cancer Society, the largest single annual drop in cancer deaths was 2.2 percent from 2016 to 2017.1 New treatments such as immunotherapy and targeted therapy as well as refinements in existing radiation oncology techniques, such as stereotactic body radiation therapy (SBRT) and 3D or volumetric-modulated arc therapy (VMAT), have contributed to the decline. Unfortunately, patients still suffer the effects of toxicity to normal, healthy tissue. While proton therapy has been shown to reduce acute adverse effects2 and is generally considered safer in terms of avoiding damage to nearby healthy tissue, another treatment option may offer even more advantages: carbon ion therapy.
The National Institute of Radiological Sciences (NIRS) in Chiba, Japan, is the world’s first carbon ion therapy center. Built in in 1994, roughly 12,000 patients have been treated with carbon ion therapy, nearly a quarter of them for localized prostate cancer. Other primary sites include bone and soft tissue, head and neck, and lung cancers.3 Currently, 12 particle therapy centers in Europe and Asia are in clinical operations using carbon ion.4
Despite its potential, providing carbon ion therapy is a costly undertaking at $300 million or more to establish a center, with no current reimbursement offered in the US.
In 2015, the University of Texas Southwestern (UTSW) and University of California, San Francisco, were awarded planning grants from the National Cancer Institute (NCI) to support development of a heavy ion treatment center. Hak Choy, MD, FASTRO, professor and chair of the Department of Radiation Oncology at the UTSW Medical Center, led an international symposium on ion therapy at his institution in November 2014 with the goal to determine the direction of future investigation and development. However, while the NCI and the National Institutes of Health (NIH) will fund research, they do not provide funds for building a facility. Globally, all other heavy ion centers – in Germany, Japan, Austria and Italy – were initially funded by their respective governments.
UT Southwestern Medical Center is sponsoring a clinical trial to compare carbon ion to photon radiation therapy for locally advanced, unresectable pancreatic cancer (CIPHER).5 Led by principal investigator David Sher, MD, the randomized trial seeks to compare overall two-year survival rates. Patients will receive treatment at a center in Japan or Milan and will include American, European and Asian patients.
Coming to America
In November 2019, Mayo Clinic announced plans to build the first carbon ion therapy center in the US on its Jacksonville, Florida, campus. As one of the early US adopters of proton therapy, Mayo is uniquely qualified to add carbon ion therapy to its armamentarium, says Bradford Hoppe, MD, MPH, professor of radiation oncology and the medical director of Particle Therapy at Mayo Clinic Jacksonville.
“Carbon ion therapy is a treatment that was developed in the US 40 years ago but hasn’t been used here in 25 years. Mayo Clinic is well positioned to lead this new effort to bring it back to the US,” says Dr. Hoppe. “We are going to examine carbon ion therapy for cancer sites where it is known to be effective, but also explore its use in novel situations, much like we have done with proton therapy. The potential is there.”
The National Comprehensive Cancer Network (NCCN) Guidelines include carbon ion therapy as an appropriate treatment for bone sarcomas and uveal melanomas. Although bone sarcomas are rare, there is a high rate of local recurrence with radiation therapy alone; therefore, surgery is preferred when technically feasible, Dr. Hoppe explains. Yet, some bone sarcomas cannot be safely resected, such as those in lower spine or base of the skull, without causing neurological or functional damage.
“Carbon ions can cause a lot more damage within the tumor [vs photon or proton therapy], so we think it is useful in tumors thought to be more radioresistant,” says Dr. Hoppe. These include melanomas, bone sarcomas, soft-tissue sarcomas, carcinomas in the lung, hepatocellular cancer, renal and pancreatic cancer, recurrent rectal cancer, as well as non-squamous head and neck cancers such as adenoid cystic and mucosal melanomas, and recurrent rectal cancer. Similarly, carbon ion therapy may provide additional benefit in patients with local recurrence following conventional radiation, where re-irradiation may be effective.
Carbon ion therapy, in one way, is similar to proton therapy in that there is no exit dose as seen with photons or conventional external-beam radiation therapy; this allows for delivery of a more conformal treatment maximizing dose in the tumor and delivering less dose to surrounding tissue. Yet, different from proton or photon radiation, it more powerfully damages the cancer cell DNA. Dr. Hoppe likens the difference to that of a cannonball (carbon) vs a bullet (proton). Carbon creates more DNA double strand breaks and chromosomal breaks making the cell more susceptible to death.
The Technology
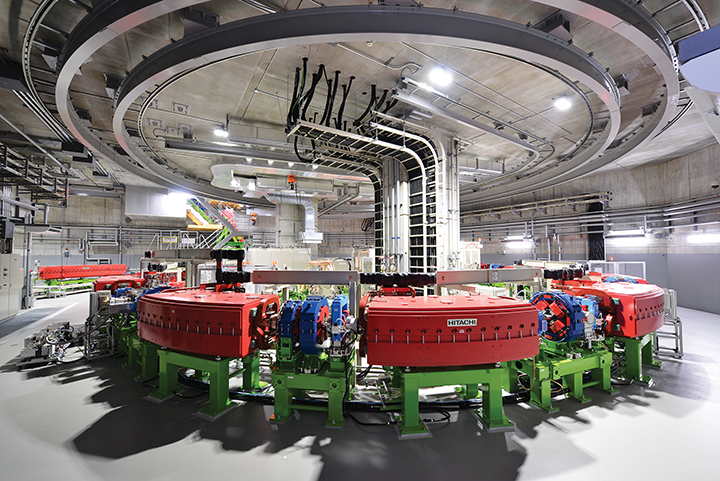
Hitachi, Ltd., has been involved with particle beam therapy solutions since 1994, including at NIRS where the company supplied the magnets, control system, beam monitors and power supply systems for the accelerator. The company’s first US-based proton beam therapy center at the University of Texas MD Anderson Cancer Center opened in May 2006. A 2017 acquisition of Mitsubishi Electric’s particle therapy equipment business has brought the company back full circle to carbon ion therapy (see Figure 1A-B for examples of a heavy ion therapy accelerator system and treatment room). Now, Mayo Clinic is partnering with Hitachi on the carbon ion therapy system in Jacksonville.
The company has also developed a compact, energy-efficient synchrotron accelerator that can power single- or multiple-room systems. This compact, single-room solution is expandable and does not require additional accelerators to power multiple rooms.
A key differentiator of Hitachi’s particle therapy system is its capability to perform both proton and carbon ion therapy. According to Sash Matsumoto, vice president of sales and marketing at Hitachi America, this hybrid particle therapy approach allows centers to start with protons and expand to carbon ion.
“Because carbon is 12 times heavier than hydrogen, it requires larger-sized equipment, which increases the construction costs,” Matsumoto says. “We believe in this technology and will continue to invest and build these centers.”
RaySearch Laboratories also supports and has invested in carbon ion therapy. RayStation Carbon Ion Therapy is a pencil-beam scanning planning system currently used by six centers in Europe and Asia.6
With several NCI-funded studies comparing proton therapy with conventional radiation therapy,7 the next logical step is comparing proton therapy with carbon ion therapy. Mayo Clinic will be well positioned to carry out this research in the US.
Mayo’s particle therapy center will have two proton gantries that will move 360 degrees around the patient and one fixed room that can perform both proton and carbon ion therapy. It is also possible that patients may receive a hybrid proton/carbon ion treatment in the fixed room.
“We don’t yet fully understand the radiobiologic effect within the target or just outside the target in normal tissue with carbon ion therapy, which means we don’t understand it in normal tissue,” says Dr. Hoppe. Theoretically, carbon ion therapy could be used to treat the center of the gross tumor volume and then proton used to treat the subclinical disease and margins because of the understanding of the radiobiology and associated toxicity to normal tissue with proton therapy.
Carbon therapy can also shorten treatment times, Dr. Hoppe adds. In unresectable bone sarcomas, the treatment time with carbon ion is half that of photon or protons.
“Carbon ion therapy can reduce treatment times by 25 to 50 percent, which may help offset some of the expense of treatment,” he says. However, since the center will not be built until 2025 and likely begin treatments in 2027, many decisions remain on precisely how Mayo Clinic will utilize carbon ion therapy.
Meanwhile, Mayo Clinic is collaborating with other carbon ion centers in Asia and Europe to embark on preclinical and clinical studies before the Jacksonville center is built. With Mayo Clinic having multiple cancer treatment centers across the US, Dr. Hoppe sees an opportunity to initiate early studies through internal referrals. He is hopeful that other US-based cancer centers will invest in carbon ion therapy and collaborate with Mayo in both pre-clinical and clinical studies in part to achieve a baseline of evidence needed for clinical use.
Also on the horizon: particle ion therapy centers exploring the potential of helium – a lighter particle than carbon yet heavier than protons – for cancer treatment. University Hospital Heidelberg, a heavy particle center in Germany, is researching helium as an alternative to proton therapy by comparing treatment plans via computer simulation.8
References
- American Cancer Society. Major cancer types: Lung, breast, prostate, and colorectal cancer. Accessed January 14, 2021. https://www.cancer.org/latest-news/facts-and-figures-2020.html#:~:text=The%2026%2Dyear%20decline%20in,in%20early%20detection%20and%20treatment
- Baumann BC, Mitra N, Harton JG, et al. Comparative effectiveness of proton vs photon therapy as part of concurrent chemoradiotherapy for locally advanced cancer. JAMA Oncol. 2020;6(2):237-246. doi: 10.1001/jamaoncol.2019.4889. PMID: 31876914; PMCID: PMC6990870
- Mohamad O, Makishima H, Kamada T. Evolution of carbon ion radiotherapy at the National Institute of Radiological Sciences in Japan. Cancers (Basel). 2018;10(3):66. doi:10.3390/cancers10030066
- Particle Therapy Co-Operative Group. Particle therapy facilities in clinical operation (last update: January 2021). Accessed January 20, 2021. https://www.ptcog.ch/index.php/facilities-in-operation
- NIH, US National Library of Medicine. Trial of Carbon Ion Versus Photon Radiotherapy for Locally Advanced, Unresectable Pancreatic Cancer (CIPHER). Accessed January 20, 2021. https://clinicaltrials.gov/ct2/show/NCT03536182
- RaySearch Laboratories. RayStation Carbon Ion Therapy. Accessed January 15, 2021. https://www.raysearchlabs.com/carbon-ion-therapy-treatment-planning
- National Cancer Institute. Is Proton Therapy Safer than Traditional Radiation? Accessed January 20, 2021. https://www.cancer.gov/news-events/cancer-currents-blog/2020/proton-therapy-safety-versus-traditional-radiation
- Tessonnier T, Mairani A, Chen W, et al. Proton and helium ion radiotherapy for meningioma tumors: a Monte Carlo-based treatment planning comparison. Radiat Oncol. 2018;1(2). https://doi.org/10.1186/s13014-017-0944-3
Citation
MB M. From Bullet to Canon? Exploring the Promise of Heavy Particle Ion Therapy. Appl Radiat Oncol. 2021;(1):46-48.
March 30, 2021