External-beam Radiation Therapy for Aspergilloma-associated Hemoptysis
Images




CASE SUMMARY
A 51-year-old man with an extensive history of left lung aspergilloma and hemoptysis was referred to radiation oncology for treatment-refractory hemoptysis. His past medical history included hypertension, multiple surgeries for congenital coarctation of the aorta, and bronchiectasis. A diagnosis of aspergilloma in the left upper lobe was made in the mid-1990s and the patient experienced bouts of hemoptysis intermittently ever since. The aspergilloma had been treated with multiple rounds of antifungal medications, including intravenous and intracavitary itraconazole, amphotericin and voriconazole. Computed tomography scans demonstrating aspergilloma in the left upper lobe are shown in Figure 1.
Prior to a consultation with radiation oncology, all standard-of-care options had been exhausted. He remained on voriconazole with no improvement of his hemoptysis. Further surgical efforts were precluded due to a descending aortic graft being plastered to the left hilum from his previous aortic surgeries. Interventional radiology was unable to embolize the left bronchial artery. Based on previous case reports describing the use of external-beam radiation therapy in treating hemoptysis secondary to fungal infection of the lung, the patient was referred to radiation oncology.
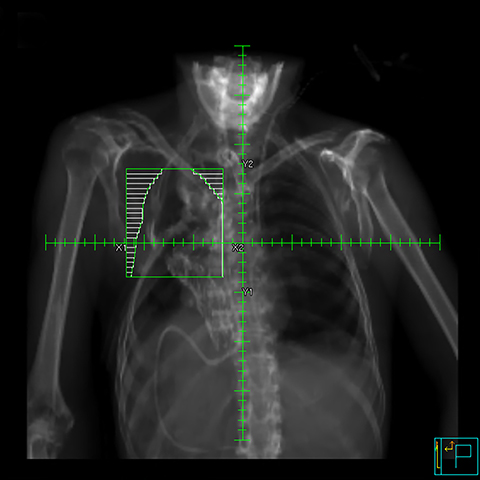
The mycetoma was contoured as the gross tumor volume (GTV). The clinical target volume (CTV) was defined as the GTV plus a 1-cm uniform expansion. To account for variation in setup and penumbra, a 1-cm margin was added to the CTV to establish the field edges. Radiation was delivered by a two-beam opposed-oblique technique at a dose of 7 Gy at 3.5 Gy per week, prescribed to the midplane with 6 MV photons (Figure 2). It was our intention to repeat the treatment every 7 days until hemoptysis resolved. The anterior and posterior beams were designed to cover the CTV with multileaf collimators set to spare healthy lung and extrapulmonary tissue. The first treatment was well tolerated and the hemoptysis resolved over the following week. A second dose was delivered to improve durability of effect. The patient was discharged after several days of monitoring.
Four months after receiving radiation therapy, voriconazole was discontinued because of apparent liver toxicity. Three months later, the patient experienced a recurrence of hemoptysis with a superimposed pseudomonas infection. This improved on oral ciprofloxacin. Several months later, he was readmitted to the hospital for worsening respiratory status despite oral ciprofloxacin and was treated with intravenous ertapenem. The patient improved after 6 days on intravenous antibiotics and was discharged home. Unfortunately, he died two weeks later after recurrence of massive hemoptysis.
IMAGING FINDINGS
Computed tomography scans of the aspergilloma in the upper lobe reveal a soft-tissue mass surrounded by air.
DIAGNOSIS
Pulmonary aspergilloma causing hemoptysis
DISCUSSION
Pulmonary aspergilloma is a condition in which Aspergillus fungi, immune cells and debris form a mass in the lung. This can develop in patients with predisposing conditions such as tuberculosis, cancer and bronchiectasis.1 The standard treatment for aspergilloma-associated hemoptysis includes pharmacologic therapies, surgical removal of the affected area and, more recently, embolization strategies.2 Surgical resection, however, requires that the patient be sufficiently healthy to endure the procedure and can be accompanied by high morbidity and mortality. Furthermore, the efficacy of embolization procedures is often transient and drug therapies may not be sufficient in many cases.1 For patients who fail these treatments, options are limited.
External-beam radiation therapy is accepted as the standard of care for palliation in patients with hemoptysis secondary to lung cancer.3 Radiation has been shown to be effective at promoting coagulation, thereby stopping bleeding in multiple sites of malignancy including the lung.4 The mechanism of how radiation promotes resolution of hemoptysis in benign diseases such as aspergilloma is unclear. It has been suggested that radiation affects the small blood vessels surrounding the mycetoma rather than the fungal ball itself, promoting swelling, necrosis and thrombosis.5
This case contributes to a nascent body of literature suggesting a role for radiation in this context. A 1980 case report was published detailing the treatment of a single patient with hemoptysis following allergic bronchopulmonary aspergillosis and aspergilloma using an initial dose of 20 Gy followed by another 10 Gy on relapse.6 A more recent report in 2011 described resolution of hemoptysis with radiation in a woman diagnosed with an aspergillosis mycetoma that was refractory to standard-of-care treatments. In this case, a cumulative dose of 28 Gy at 3.5 Gy per fraction delivered weekly was used, similar to the regimen used in our case.7
Reports involving multiple patients are sparse. In a 5-patient series for patients with a history of hemoptysis who were ineligible for standard-of-care therapies, patients were treated with varying cumulative doses of radiation therapy ranging from 7 to 14 Gy depending on the dose required to sustain symptom alleviation delivered at 3.5 Gy per fraction weekly. This appeared safe and effective at 6-month follow-up.5 We followed this regimen, delivering 3.5 Gy per fraction weekly until symptom alleviation. Two of the patients in this series required 7 Gy to resolve hemoptysis as did our patient, while others required a higher dose to achieve resolution. It is unclear whether a higher dose produces a more durable response in patients who experience symptom relief at a lower dose. A single-institution retrospective analysis of 21 Brazilian patients who received radiation therapy for aspergilloma-mediated hemoptysis following a diagnosis of tuberculosis demonstrated a failure-free survival rate of 82%.8 Patients received 2 Gy daily up to 34 Gy, with most patients receiving 20 Gy via a cobalt-60 source. This was the only case series with follow-up > 8 months (median 25 months), making estimated duration of benefit unclear.
While the aforementioned reports suggest that external-beam radiation therapy shows potential in treating hemoptysis following aspergilloma, we are limited by the small number of patients studied and the lack of a standardized dosing regimen. The studies describe different dosing regimens and sometimes were forced to adjust doses depending on patient response. Even in hemoptysis secondary to malignancy, controversy remains regarding optimal radiation dosing.9 This fact as well as the experience described herein highlight the need for larger-scale studies to optimize delivery of these treatments to realize their full potential. Currently, one randomized early phase clinical trial (NCT02878447) is aiming to recruit 40 patients with hemoptysis following aspergillomata, and we await how these results will inform the management of this rare, difficult-to-treat condition.10 This trial uses the same fractionation scheme as our case, and treats all affected lung tissue. Until we have more evidence to guide practice, proper patient selection and consent will be important in this novel use of radiation.
CONCLUSIONS
We present the case of a 51-year-old man with treatment-refractory aspergilloma-related hemoptysis who received a total of 7 Gy in 2 fractions delivered weekly and had resolution of his hemoptysis. Seven months after discharge, hemoptysis recurred, and the patient died. We demonstrate that while this treatment modality shows promise for benign causes of hemoptysis, our current state of knowledge is limited. Future studies will be important to guide proper patient selection and optimal dosing.
REFERENCES
- Kousha M, Tadi R, Soubani AO. Pulmonary aspergillosis: a clinical review. Eur Respir Rev. 2011;20(121):156-174.
- He G, Liu W, Gao Z, Gao Z, Gao H, Wang Y. Intervention treatment on massive hemoptysis of pulmonary aspergilloma. Exp Ther Med. 2017;13(5):2259-2262.
- Rodrigues G, Videtic GMM, Sur R, et al. Palliative thoracic radiotherapy in lung cancer: an American Society for Radiation Oncology evidence-based clinical practice guideline. Pract Radiat Oncol. 2011.
- Rasool MT, Manzoor NA, Mustafa SA, Maqbool LM, Afroz F. Hypofractionated radiotherapy as local hemostatic agent in advanced cancer. Indian J Palliat Care. 2011.
- Falkson C, Sur R, Pacella J. External beam radiotherapy: a treatment option for massive haemoptysis caused by mycetoma. Clin Oncol. 2002;14(3):233-235.
- Shneerson JM, Emerson PA, Phillips RH. Radiotherapy for massive haemoptysis from an aspergilloma. Thorax. 1980;35(12):953-954.
- Samuelian JM, Attia AA, Jensen CA, Monjazeb AM, Blackstock AW. Treatment of hemoptysis associated with aspergilloma using external beam radiotherapy: a case report and literature review. Pract Radiat Oncol. 2011;1(4):279-281.
- Sapienza LG, Gomes MJL, Maliska C, Norberg AN. Hemoptysis due to fungus ball after tuberculosis: a series of 21 cases treated with hemostatic radiotherapy. BMC Infect Dis. 2015.
- Ma JT, Zheng JH, Han CB, Guo QY. Meta-analysis comparing higher and lower dose radiotherapy for palliation in locally advanced lung cancer. Cancer Sci. 2014.
- University of Stellenbosch. The utility of radiotherapy in the management of haemoptysis secondary to aspergillomata and structural lung diseases.
Citation
DJ B, AJ A, BP Y. External-beam Radiation Therapy for Aspergilloma-associated Hemoptysis. Appl Radiat Oncol. 2020;(1):40-42.
April 4, 2020