Brachytherapy for Resistant Disseminated Superficial Actinic Porokeratosis
Images





CASE SUMMARY
A 61-year-old Caucasian woman with a past medical history of hidradenitis suppurativa and Hashimoto’s thyroiditis presented with a 15-year history of disseminated superficial actinic porokeratosis (DSAP) on her bilateral legs and forearms. Previous treatments for her DSAP have included photodynamic therapy (PDT), cryotherapy, and imiquimod with no improvement. Physical examination revealed diffuse subcentimeter to centimeter papules on her bilateral legs and forearms (Figure 1A). Because of failure with previous treatments, high-dose-rate iridium-192 brachytherapy (HDR-BT) was delivered to a small lesion on the left leg with plans to perform wider spread treatment if this course was successful. This lesion was chosen due to its small size, accessibility to the applicator, and because any changes in the lesion could be readily observed and verified. In addition, this DSAP lesion was adjacent to a lentigo, which would allow for quick identification at subsequent treatment sessions and follow-ups. A total of 20 Gy in 4 fractions of 5 Gy each was delivered (1 fraction per week) using a 3.0 cm Leipzig applicator with a Varisource Afterloader (Varian). The dose was prescribed at surface (0 mm depth). No side effects were noted other than mild hyperpigmentation, which arose in the treated area 1 to 2 weeks after the start of treatment (Figure 1B). At 4 months post-treatment, there was resolution of the DSAP papule (Figure 1B). At 10 months post-treatment, there was persistent faint hyperpigmentation in the treated area with no clinical reoccurrence of the DSAP lesion.
IMAGING FINDINGS
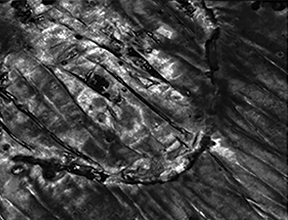
An untreated area on the same leg revealed atrophic papules with a circumferential hyperkeratotic rim under dermoscopy (Figure 2A), while dermoscopy of the treated area showed no remaining hyperkeratosis (Figure 2B). Reflectance confocal microscopy (RCM) of the untreated site revealed mild inflammation, well-defined focal parakeratosis in the epidermis (cornoid lamellation), focal atypia of keratinocytes, and several dilated blood vessels in the dermis (Figure 2C), while the treated site had absent cornoid lamellation, with only dendritic cells at the dermal-epidermal junction, and mild spongiosis present (Figure 2D).
DIAGNOSIS
Physical examination as well as dermoscopic and RCM findings were consistent with a diagnosis of DSAP.
DISCUSSION
Porokeratosis describes six chronic progressive conditions of disordered keratinization that lead to pruritus, cosmetic distress and, occasionally, malignant transformation.1 Porokeratotic lesions begin as red to brown papules with raised borders that may coalesce to form plaques. DSAP is one of the six variants of porokeratosis, including linear porokeratosis, porokeratosis of Mibelli, punctate porokeratosis, porokeratosis palmaris et plantaris disseminata, and nonactinic disseminated superficial porokeratosis.2 DSAP lesions are distinguished by their late onset and prevalence in sun-exposed areas while sparing the palms and soles.1 Most commonly, DSAP occurs in fair-skinned women between 30 and 50 years old, and risk factors include genetics, immunosuppression, and sun exposure.1 The incidence and prevalence of DSAP is unknown; however, in the US, it is classified as an orphan disease.3 There is a 7.5% to 10% risk of malignant transformation to squamous cell carcinoma (SCC) or basal cell carcinoma (BCC).2
The histology of DSAP is characterized by parakeratotic cells arranged around a circumferential ridge called a cornoid lamella.1 The cornoid lamella distinguishes DSAP from other cutaneous lesions found on sun-exposed sites such as actinic keratosis (AK) and SCC.1 Conventional histology requires biopsy of the lateral border of a DSAP papule, while RCM provides a precise and noninvasive view of different skin layers in vivo. Under RCM, DSAP papules have demarcated hyper-refractile borders in the corneal layer, cellular and nuclear atypia at the spinous and granulosa layers, and dilated blood vessels and lymphatic infiltrates at the upper dermis.4
While the aesthetic appearance and therapeutic resistance of this condition has a significant psychosocial and economic burden, there remains no standard or effective treatments for DSAP. Only variable improvement has been shown with imiquimod, 5-fluorouracil PDT, vitamin D, retinoids, and lasers.1 Due to recent advancements in safety, superficial radiation therapy (RT) is gaining popularity for the treatment of unresectable skin tumors and benign dermatoses.5 While earlier reports document the development of porokeratosis in cancer patients treated with RT, it remains unclear whether the development resulted from impaired immunity or DNA-damaging cotreatments.6 Grenz rays (GR), a low-energy form of x-ray therapy, has been used to successfully treat DSAP, but the use of GR remains controversial due to a 1989 study warning of the risk of secondary skin cancer development following this treatment.7 However, this report has been disputed as an overestimate of this risk due to conflations of GR with other forms of superficial radiation and superficial x-ray therapy.8,9 Long-term follow-up (15 years) of 14,140 patients who received GR therapy for benign conditions reported only 58 cases of malignant skin tumors, each diagnosed more than 5 years after GR therapy had first been administrated. Of that group, 19 patients had malignant melanomas and 39 patients had other malignant skin tumors.10 Only 8 of those with malignant tumors had received GR at the site of their secondary malignancy and 6 of those 8 had exposures to other known carcinogens.10
HDR-BT is another form of superficial radiation therapy that involves the application of radionuclides in or near a tumor. Treatment diameter reduction and added shielding to HDR-BT have allowed for the safer delivery of superficial radiation to the skin especially in benign conditions such as keloids.11 Previous studies have examined safety outcomes 10 years after HDR-BT treatment in 520 patients treated SCC, BCC, melanoma, paraneoplastic skin manifestations, and keloids.12 Of these patients, 91% obtained complete remission with no severe late reactions.12 A similar study of 200 patients who received HDR-BT for SCC and BCC concluded that HDR-BT provided good to excellent cosmesis (88%), low recurrence (2%), and no significant acute or long-term skin toxicities after 25 to 121 months.5 Thus, similar to GR, HDR-BT offers limited penetration and does not carry a significant risk for secondary skin malignancies. However, HDR-BT may cause long-term side effects such as mild hypo- or hyperpigmentation, hair loss, fibrosis and telangiectasias in the treated area. Other limitations of the use of HDR-BT for the treatment of DSAP may include cost, amount of body surface area involved, age, a patients’ other medical history, and risk of secondary malignancy.13
CONCLUSION
This case demonstrates that HDR-BT can be an effective treatment for resistant DSAP to a selective area. Dermoscopy of the treated area showed no remaining hyperkeratosis, and RCM demonstrated absence of the cornoid lamellation, characteristic of DSAP. Due to the significant cosmetic distress and lower malignant transformation of this condition, HDR-BT may be a reasonable therapy in patients who have failed conservative treatments. However, further large-scale studies are needed to determine the long-term safety, efficacy, and practicality of HDR-BT use in DSAP.
REFERENCES
- Skupsky H, Skupsky J, Goldenberg G. Disseminated superficial actinic porokeratosis: a treatment review. J Dermatolog Treat. 2012;23(1):52-56.
- Le C, Bedocs PM. Disseminated superficial actinic porokeratosis. StatPearls [Internet]. StatPearls Publishing; 2019.
- Kanitakis J. Disseminated superficial actinic porokeratosis. 2015; Accessed April 29, 2020. https://www.orpha.net/consor/cgi-bin/OC_Exp.php?Lng=GB&Expert=79152
- Ulrich M, Forschner T, Röwert-Huber J, et al. Differentiation between actinic keratoses and disseminated superficial actinic porokeratoses with reflectance confocal microscopy. Br J Dermatol. 2007;156 Suppl 3:47-52.
- Gauden R, Pracy M, Avery A-M, Hodgetts I, Gauden S. HDR Brachytherapy for superficial non-melanoma skin cancers. J Med Imag Radiat Oncol. 2013;57(2):212-217.
- Romani J, Pujol RM, Casanova JM, de Moragas JM. Disseminated superficial porokeratosis developing after electron-beam total skin irradiation for mycosis fungoides. Clin Exp Dermatol. 1996;21(4):310-312.
- Burns FJ. Cancer risk associated with therapeutic irradiation of skin. Arch Dermatol. 1989;125(7):a979-981.
- Gladstein AH. Dermatologic radiation and cancer. Arch Dermatol. 1990;126(1):120-121.
- Kingery FAJ, Russell PS, Larsen WG. Safety of Grenz Ray Therapy. Arch Dermatol. 1990;126(1):119-120.
- Lindelof B, Eklund G. Incidence of malignant skin tumors in 14,140 patients after grenz-ray treatment for benign skin disorders. Arch Dermatol. 1986;122(12):1391-1395.
- Goutos I, Ogawa R. Brachytherapy in the adjuvant management of keloid scars: literature review. Scars Burn Heal. 2017;3:2059513117735483-2059513117735483.
- Kohler-Brock A, Prager W, Pohlmann S, Kunze S. [The indications for and results of HDR afterloading therapy in diseases of the skin and mucosa with standardized surface applicators (the Leipzig applicator)]. Strahlenther Onkol. 1999;175(4):170-174.
- Delishaj D, Rembielak A, Manfredi B, et al. Non-melanoma skin cancer treated with high-dose-rate brachytherapy: a review of literature. J Contemp Brachytherapy. 2016;8(6):533-540.
Citation
J S, S N, AB L, I K, F S, BK R, L P, IH H. Brachytherapy for Resistant Disseminated Superficial Actinic Porokeratosis. Appl Radiat Oncol. 2020;(3):43-45.
September 9, 2020