Augmenting cancer control efforts in a limited resource setting by leveraging international collaborations in radiation oncology
Images

SA-CME credits are available for this article here.
Cancer remains an important cause of morbidity and mortality globally with incidences projected to rise in the coming decade. Nearly two-thirds of these new cases are anticipated to be recorded in low- and middle-income countries (LMICs) such as Ghana, where infectious diseases remain a major public health challenge.1,2 More than 70% of cancer patients in low-income countries are expected to die from their disease compared to about 30% in Western countries.3
It is estimated that about half of cancer patients would require radiation therapy (RT) as part of their care.4 In under-resourced environments where screening and early detection programs are almost nonexistent and a large proportion of patients present with advanced disease, optimum RT utilization to improve local disease control and to palliate cancer-related distressing symptoms is estimated to be high.5 However, the availability of these services is far less than desirable in these LMICs.5,6 RT is estimated to contribute about 40% toward the curative treatment of cancer,7 and accounts for only 5% of the total cost of care in Sweden.8 The unavailability of radiation treatment, therefore, becomes a universal health coverage issue of equity, quality and financial risk for most LMICs.
In this review, we describe the current status of RT in Ghana, West Africa, and explore innovative international collaborative efforts aimed at addressing unmet needs and improving radiation treatment for patients.
Patients
Approximately 3500 new adult and pediatric patients are seen annually at the 3 RT centers in Ghana.9 The Radiotherapy Centre at Korle Bu Teaching Hospital (KBTH), for instance, sees approximately 1600 patients per year, and the 5 most common cancers seen are breast (27.7%), prostate (11.9%), cervix (8.3%), bone marrow (4.3%), sarcoma (38%) and lung (3.5%), according to current institutional records. Optimum and actual RT utilization for Ghana are 51% and 9%, respectively.9 Several reasons may attribute to this low patronage, including paradigm-to-disease causation, complementary and alternative medicine use,10 number of megavoltage machines per million people and their distribution (Figure 1), health literacy and financing.
Equipment/Services
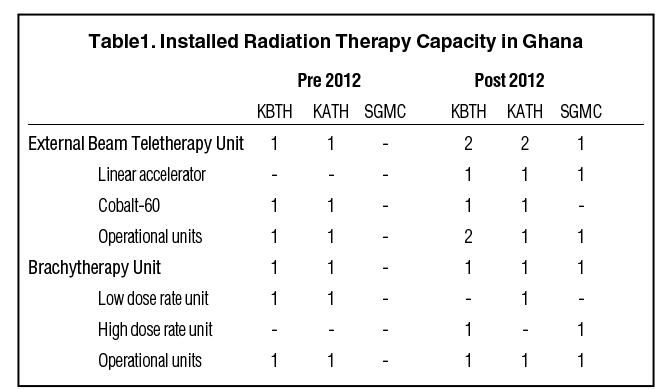
Ghana has made modest gains in improving access to RT services in recent years (Table 1). The nation has 3 RT centers, 2 of which are public, and the third private (a joint Sweden-Ghana partnership). Two of the facilities are in Accra—the KBTH and Sweden Ghana Medical Center (SGMC)—and the third is in the Komfo Anokye Teaching Hospital (KATH), Kumasi. The establishment of SGMC has been an excellent addition to the repertoire of treatment options. There are currently 3 modern cobalt-60 teletherapy machines at the 2 government-owned centers (KATH and KBTH), and 3 linacs in the country (5 megavoltage units in total). These consist of a 6-MV and 15-MV linac with electron therapy at SGMC, a newly commissioned 6-MV linac with intensity-modulated radiation therapy (IMRT) and volumetric-modulated arc therapy (VMAT) in Korle Bu, and a dual-photon energy linac (6 and 15 MV with electrons) in Kumasi yet to be commissioned. By international standards, Ghana requires 22 MV machines for its 30 million inhabitants for full access, 12 hours a day.11
Cobalt-60 is utilized for cervical high dose rate (HDR) brachytherapy since it is more cost effective, requiring a less frequent source change. The 2 cobalt external-beam radiation therapy machines have proven useful in the past 20 years—indeed several patients have been cured on the cobalt.12,13 It is a relatively simple machine compared to the linear accelerator and, therefore, has simple quality control and assurance protocols, and by extension requires less sophisticated expertise to keep running. It is also relatively cheap. Source change protocols may, however, be challenging, as is the dosimetry for deep-seated tumors and very superficial tumors in the absence of VMAT and electrons.
Radioiodine treatment for thyroid cancer is available at the National Radiotherapy Oncology and Nuclear Medicine Center (NCRONM). NCRONM also performs prostate brachytherapy using iodine-125 low dose rate (LDR) brachytherapy. The isotopes are ordered as required. The LDR prostate brachytherapy program has been made possible through collaborative work between KBTH and Bard Medical (Covington, Georgia).14
Radiotherapy Workforce in Ghana
Ghana has training programs for all cadre of staff required for radiation therapy delivery including oncologists, medical physicists, radiation therapy technologists (RTTs) and biomedical engineers. Currently, there are 12 oncologists and 10 residents in training, 13 physicists, 27 RTTs, 7 engineers, and 59 nurses. These mainline staff work together to serve patients referred to the oncology centers.
Oncologists. Doctors specializing in oncology in most African countries function as both radiation and medical oncologists (clinical oncologists) and, therefore, receive appropriate training for this. In Ghana, oncologists are trained at the Ghana College of Physicians and Surgeons. The training program is in 2 phases—the initial membership phase is a 4-year program followed by a 2-year fellowship, culminating in the award of fellow of the college. To maximize efficiency in patient care as well as personnel expertise, clinics are run based on disease sites on specific days of the week. The NRONMC often experiences heavy clinical workload, which includes extended consulting hours, brachytherapy procedures, patient simulation, tumor volume delineation and treatment planning. More recently, the introduction of a patient appointment system has streamlined patient scheduling.
Medical physicists. Medical physicists play a vital role in the entire process of planning and execution of radiation treatment within a radiation facility. Training of medical physicists in Ghana entails a 2-year master of science degree and 2-year internship with the School of Nuclear and Allied Sciences, University of Ghana. A prerequisite for admission into the program is a bachelor of science degree in physics. All of the medical physicists have a master of science degree and 1 recently completed a PhD program. The physicists also function as dosimetrists and execute both roles favorably and are involved in regular quality assurance and quality control procedures. They are actively involved in acceptance testing and commissioning of new RT equipment with acquisition of beam data, as was done when the new linacs were commissioned. The dosimetry was validated by medical physicists from the equipment vendors. Physicists participate in brachytherapy planning (cervical and prostate) in conjunction with physicians, and coordinate and monitor the use of radioiodine therapy. The physicists calibrate suitable scanners outside the hospital to acquire DICOM images for treatment planning, and an in-house computed tomography (CT) scanner is under installation. Of note, another pivotal role of the physicists is collaborating with external manufacturing engineers to report machine malfunctioning and assist in diagnosis and repair of minor faults on the machines.
Radiation Therapy Technologists. RTTs constitute an essential workforce in any RT facility. A 4-year training program with a 1-year internship under the Department of Radiography, School of Biomedical and Allied Health Science, College of Health Sciences at the University of Ghana is available for training RTTs. RTTs treat patients, perform treatment verification, conduct 2-Dimensional (2D) simulation, and provide final simulation after 3-dimensional (3D) treatment planning, as well as molding of custom-made blocks for treatment on the cobalt unit. RTTs also accompany patients who are due for 3D treatment planning to CT facilities outside the hospital to have their scans done according to RT specification with a flat-panel insert into the couch. The newly acquired linear accelerators have multileaf collimators, obviating the use of Cerrobend blocks. RTTs run 2 shifts daily at NCRONM to ensure respectable waiting times.
Biomedical engineers. Biomedical engineers play a significant role in keeping imaging and treatment machines functioning optimally. In NRONMC there are 4 trained engineers: 2 with a 4-year bachelor of engineering degree and the others with a higher national diploma who handle most problems on the RT machines. Equipment manufacturing companies provide backup support for the linear accelerator in conjunction with the on-site engineers and physicists. Warranty issues require engineers from equipment vendors to address certain problems, and there is room for improvement regarding response time.
Nursing. Alongside doctors, specially trained oncology nurses at the NRONMC and the other centers in the country are directly involved in patient management regarding administration of systemic therapy and RT-related nursing services. A significant number of patients receive concurrent or sequential chemotherapy and occasionally targeted therapy. The importance of coordinating chemotherapy administration and RT cannot be overemphasized. Our nurses continually play a vital role in this regard even though they are tasked with the care of large numbers of patients requiring chemotherapy. Furthermore, they take on the additional responsibility of optimally scheduling patients on the treatment machine who are receiving concurrent chemotherapy. Nurse navigation has been introduced over the last few years to ensure the optimal care of patients through treatment and proper handling of any concerns that may arise. With the graduation of the first batch of 3 oncology nurse specialists/practitioners from the Ghana College of Nurses and Midwives last year after a 3-year training program, and ongoing training of more nurses in this specialized capacity, it is believed that patient care will dramatically improve in the ensuing years.
Quality Assurance
These limitations have not impeded progress in ensuring a relatively smooth workflow in the radiation centers in Ghana. The challenges are often mitigated by the excellent coordination between doctors, physicists and RTTs in the process of planning, verification, and treatment. The implementation of departmental clinical quality assurance meetings and weekly multidisciplinary tumor boards in breast, head and neck, and pediatric cancers have markedly improved communication between the staff and enhanced patient care. This process improvement is especially noteworthy considering the tight patient schedules and heavy clinical load. Additionally, doctors and residents engage in clinical didactics, journal club meetings, and continuing professional development programs, and attend national and international conferences throughout the year to learn about pertinent advancements in the field. Another significant activity is the participation by some Ghanaian oncologists (members of the African Cancer Coalition) in the ongoing harmonization of the National Comprehensive Cancer Network guidelines for Sub-Saharan African countries under the American Cancer Society.15
Additionally, a radiation safety officer ensures compliance with regulations set out by the country’s nuclear regulatory authority. Ghana also participates regularly in International Atomic Energy Agency/World Health Organization (IAEA/WHO) postal dose audits.16
Collaboration Efforts in Capacity Building
The radiation centers in Ghana actively partner with several upper-middle income countries to foster cancer research and training institution. One example is a thriving collaboration between the Moffitt Cancer Center (MCC), KBTH and SGMC. In 2016, Drs. Yarney and Yamoah mentored a radiation oncology resident from MCC who received the prestigious ARRO-ASTRO Global Health Fellowship award to support a research elective at KBTH to study prostate and cervical cancer. While there are no training collaborations in cancer research between Ghana and MCC, cancer research training and capacity building are under active discussion. This has given birth to the first research fellowship program at MCC, designed to host a Ghanaian radiation oncology fellow for 1 year, which began in the 2018-2019 academic year. The fellow is learning skills to facilitate future collaborations between the radiation oncology program at MCC and Ghana. This fellowship program comes at a crucial time in the development of training and capacity-building programs in Ghana. Through this collaboration, the KBTH and MCC will continue to explore other funding opportunities in cancer research training to allow Ghana to expand its expertise for an independent cancer research infrastructure. Residents also receive an annual compressed didactic course in radiobiology from faculty at MCC.
In addition, mentorship programs with the University of Toronto (Princess Margaret Cancer Center) partner residents with faculty on a 1-year research question as well as a 12-week program using telehealth-facilitated knowledge transfer in clinical decision-making, biostatistics, and quality assurance in RT. Some of these collaborations have resulted in several publications.13,17–19
KATH and its oncology directorate have had extensive and continuing engagement with the University of North Norway on a breast health global initiative to revive pathology services. Pathology is central in oncology decision-making, and this collaboration has resulted in tremendous improvement in reporting on breast as well as other cancers. The University of Michigan has also partnered with KATH on breast cancer care and regularly participates in its weekly telemedicine multidisciplinary meeting.17 The National Cancer Institute, Bethesda, Maryland, has also offered training in cancer epidemiology and advanced epidemiology for a number of participants from Ghana over the past few years.
Furthermore, the IAEA organizes at least 3 training programs a year for member states on common cancers in Africa, occasionally including expert missions and scientific visits as well as training on the management of RT centers. Ghana has taken advantage of these ongoing programs, which have been highly beneficial.
Research and Training in Ghana
To ensure a more sustainable and long-term impact in global health initiatives in Ghana and other LMICs, research and training needs to be integrated into an collaborative partnership by focusing on the following strategic goals: First, training and capacity building should center on conducting research on cancers of common interest to both parties. Second, the cancer research training initiatives must be designed in the context of existing research collaborations within the local oncology centers, thus seamlessly complementing ongoing efforts in Ghana. Currently collaborative activities initiated between MCC and KBTH include 1) providing health professionals with knowledge and tools in research methodologies for the management and use of medical information and abstraction and 2) providing health professionals, staff, oncology residents, fellows, and students with access to MCC’s expertise in clinical research methodologies, biostatistics, management of medical information, manuscript writing for publication, and grant writing. Together, these efforts are expected to help fill the gaps and address specific needs outlined in the national cancer research agenda.
Future Directions
Ghana demonstrates that a country with limited resources and obvious challenges is capable of growth and success with the ability to overcome setbacks and harness innovation in the face of limitation. Positive leadership and high-level support cannot be underestimated and has resulted in the acquisition of RT facilities to meet the rising demands of the specialty and gradually bridge the gap with technological advancements. Considering the economic status of the country, coupled with other competing health and socioeconomic interests, this has not been easy to accomplish. The MOH, GAEC and IAEA have been instrumental in supporting and building the public RT centers to their present state of technological advancement. With the recent installment of 2 new linacs and an Eclipse planning system (Varian, Palo Alto, California) with additional contouring stations and an ARIA record and verify system in Accra and Kumasi, Ghana has made great strides. Additionally, the NRONMC has recently acquired a wide-bore CT simulator that is under installation.
The institution and sustenance of training programs to ensure continuing production of high-quality professionals in oncology is empirical evidence of future growth spurts in this field. Upgrading the skill of engineers to handle more sophisticated equipment and training more dosimetrists will be necessary to continue growth and development. These tasks, coupled with the Ministry of Health’s commitment to improve healthcare delivery in the country, the roll out of the national cancer control plan and growth of the cancer registry,18 will ensure that cancer treatment continues to expand and advance in Ghana. In addition, plans to start IGRT for prostate cancer treatment with gold fiducial seeds are underway. A new bunker is also being built to accommodate another linac in the near future. Further commitment, however, is required from the government to enhance radiation delivery and cancer treatment as a whole.
With ongoing human resource training and continuous improvement of logistics, equipment, and infrastructure, efforts should focus on: 1) relying on evidence-based data from population-based registries to inform policy on preventable cancers such as liver and cervical cancer; 2) developing health promotion and literacy programs on cancers; 3) promoting screening and early detection programs for prompt diagnosis and optimal treatment in a cost-effective manner; 4) decentralizing newer radiation treatment centers to improve access; and 5) continuing to foster global collaborative partnerships to address cancers of mutual interest in a multidisciplinary and multi-institutional setting.
In the near future, we believe we will put ourselves in a position to participate in research programs undertaken by cooperative oncology research networks that involve multicenter, multi-institutional randomized controlled trials to answer pressing and pertinent questions in oncology, taking advantage of disparity in biology and disease distribution across the world. This can increase accrual rates and answer questions on disease characteristics that are uncommon in high-income countries.
Conclusion
As Ghana has demonstrated, innovative use of basic equipment and gradual building of capacity in a resource-limited LMIC is essential. Acquisition of RT facilities must be considered in the context of available resources with a stepwise approach to increasing capabilities and complexity. This has obviously been an evolutionary process that continues to unfold with time. With general improvements in outcomes of cancer treatment worldwide, patients in LMICs are living longer and quality of life is becoming a real priority. Maximum benefit can only be realized with universal health care.
References
- Boutayeb A. The double burden of communicable and non-communicable diseases in developing countries. Trans R Soc Trop Med Hyg. 2006;100:191-199.>
- Bygbjerg IC. Double burden of noncommunicable and infectious diseases in developing countries. Science. 2012;337:1499-1501.
- Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: Cancer J Clin. 2018;68:394-424.
- Slotman BJ, Cottier B, Bentzen SM, et al. Overview of national guidelines for infrastructure and staffing of radiotherapy. ESTRO-QUARTS: work package 1. Radiother Oncol. 2005;75(3):349-354.
- Zubizarreta E, Fidarova E, Healy B, et al. Need for radiotherapy in low and middle income countries–the silent crisis continues. Clin Oncol. 2015;27:107-114.
- Delaney GP, Barton MB. Evidence-based estimates of the demand for radiotherapy. Clin Oncol. 2015;27:70-76.
- Barnett GC, West CM, Dunning AM, et al. Normal tissue reactions to radiotherapy; towards tailoring treatment dose by genotype. Nat Rev Cancer. 2009;9:134-142.
- Ringborg U, Bergquist D, Brorsson B et al. The Swedish Council on Technology Assessment in Health Care( SBV) systemic review of radiotherapy including a prospective survey of radiotherapy practice in Sweden 2001--Summary and Conclusions. Acta Oncol. 2003;42:357-365.
- Rosenblatt E, Fidarova E, Zubizarreta EH, et al. Radiotherapy utilization in developing countries: an IAEA study. Radiother Oncolog. 2018;128(3):400-405.
- Yarney J, Donkor A, Opoku SY, et al. Characteristics of users and implications for the use of complimentary and alternative medicinein Ghanaian cancer patients undergoing radiation and chemotherapy: a cross-sectional study. BMC Compliment Altern Med. 2013;12:16.
- Zubizerrata E, Vandyk J, Lievens Y. Analysis of global radiotherapy needs and costs by geographic reion and income level. Clin Oncol. 2017;29(2)84-92.
- Yarney J, Aryeetey NA, Mensah A, et al. Does concurrent chemoradiotherapy preceded by chemotherapy improve survival in locally advanced nasopharyngeal cancer patients? Experience from Ghana. Cancers Head Neck. 2017;2:4.
- Vulpe H, Asamoah FA, Mangati M, et al. External beam radiation therapy and brachytherapy for cervical cancer: the experience of the National Centre for Radiotherapy in Accra, Ghana. Int J Radiat Oncol Biol Phys. 2018;100(5):1246-1253.
- Mensah JE, Yarney J, Vanderpuye V, et al. Prostate brachytherapy in Ghana: our initial experience. J Contemp brachyther. 2016;8:379.>
- Network NCC: NCCN Harmonized Guidelines, 2019.
- Sackey TA, Shirazu I, Pokoo-Aikins M, et al. The IAEA/WHO TLD Audit Program. The results of the TLD postal dosimetry audits in the National Centre for Radiotherapy and Nuclear Medicine Department, Korle-Bu, Accra (1998 to 2012). 2018.
- Jiagge E, Oppong JK, Bensenhaver J, et al. Breast cancer and African Ancestry: lessons Learned at the 10-year Anniversary of the Ghana-Michigan Research Partnership and International Breast Registry. J Global Oncol. 2016;2(5): 302-310.
- Yamoah K, Beecham K, Hegarty SE, Hyslop T, Showalter T, Yarney J. Early results of prostate cancer radiation therapy: an analysis with emphasis on research strategies to improve treatment delivery and outcomes. BMC Cancer. 2013;13:23.
- Asamoah FA, Yarney J, Awasthi S, et al. Contemporary radiation treatment of prostate cancer in Africa: a Ghanaian experience. J Gobal Oncol. 2018;4:1-13.
- Calys-Tagoe BN, Yarney J, Kenu E, et al. Profile of cancer patients seen at Korle Bu teaching hospital in Ghana (a cancer registry review). BMC Res Notes. 2014;7:577.
Citation
J Y, HA A, V V, FA A, B A, C E, S T, S D, PA S, F D, KA K, C A, B D, R W, H V, S A, A F, S W, P J, L H, L Y. Augmenting cancer control efforts in a limited resource setting by leveraging international collaborations in radiation oncology. Appl Radiat Oncol. 2019;(2):22-26.
July 11, 2019