Utilization of Decision Theory and Decision Trees to Make Treatment Choices for Postoperative Reirradiation for Recurrent HNC
Images
Abstract
The decision to pursue head and neck reirradiation after surgery is difficult given the morbidity of treatment and lack of high-quality data. Patients are then faced with the difficult decision between a low chance of cure or debilitating side effects; thus, incorporation of their values in this discussion is of paramount importance. By using decision theory and the concept of expected utility, we have created an interactive web-based decision tree in which oncologists can incorporate the best available clinical data, as well as patient values. This interactive web-based decision tree is a practical and easy-to-access solution and can be a powerful tool in the shared decision-making process.
Keywords: Head and neck cancer, reirradiation, decision theory, expected utility theory, decision trees
Case Summary
Head and neck cancer is the eighth leading cancer in men with a predicted 54,010 new cases and 10,850 deaths in 2021.1 Local recurrences or persistent disease after primary treatment occur in 17% to 40% of patients.2,3 Of these patients, those who undergo salvage surgery only have a 21% to 47% chance of living without disease or dying of other causes, and many will be considered for reirradiation.3 The morbidity from reirradiation after salvage surgery, however, can be significant with approximately a 40% chance of grade 3 or higher toxicity.4 The patient then faces the difficult decision between a low chance of cure or debilitating side effects. Compounding the difficulty, the data in this area are very complex and confusing for clinicians, let alone patients, to make clear decisions. For instance, a verbal summary of the data from the only randomized trial by Janot et al would be “if you chose reirradiation you would have approximately a 60% chance of locoregional control with a 40% chance of significant side effects and without reirradiation a 60% chance of locoregional failure and 10% of chance of side effects.”4 This is difficult for even experienced physicians to understand, yet we expect our patients to choose treatment with this information. How can we present these choices in a clearer, more scientific manner and incorporate each individual’s preferences? Decision theory is a scientific discipline dedicated toward optimizing individual choices with multiple outcomes in the face of uncertainty.5 To help overcome uncertainty, one should use the option with greatest expected desirability or value, otherwise known as “expected utility.” These expected utilities are then placed into a decision tree, which is a network governed by decision nodes (patient choices) and chance nodes that contain conditional probabilities (Figures 1 and 2).6 The other relevant portion of decision theory to oncology is the incorporation of the patient’s own desire and values when making difficult decisions.7 Only a patient can determine their own risk tolerance when balancing the chance of tumor control vs the potential morbidity of reirradiation. This paper presents an interactive web-based decision tree model (eDecision Tree in the Supplement at https://www.headandneckreirradiation.com) that incorporates uncertainty regarding tumor control and grade 3 or greater toxicity to help patients choose between uncertain payoffs and subjective risk aversions (ie, tumor control vs quality of life).8
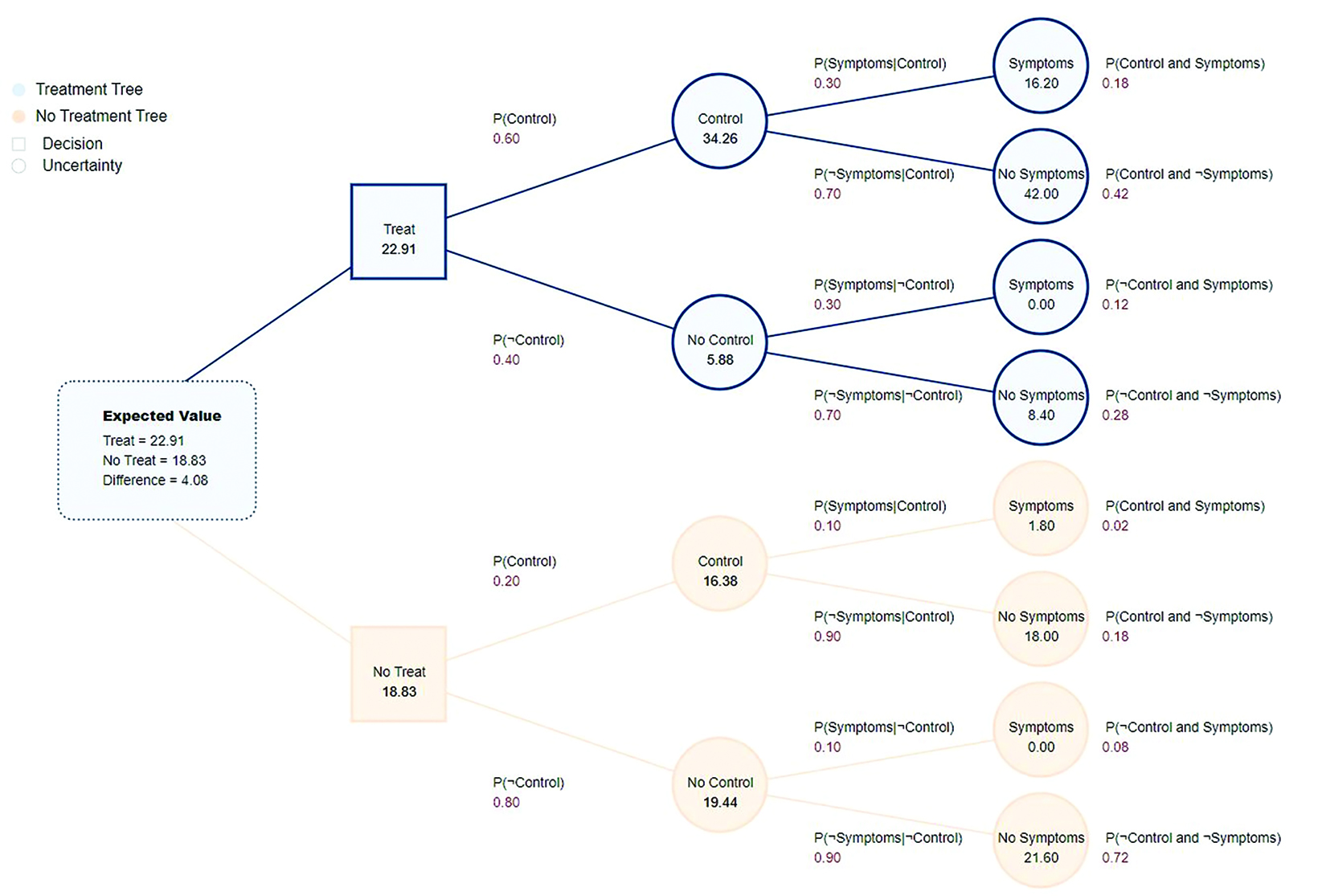
Decision trees are constructed with 2 types of nodes. The square nodes of the decision tree represent decisions the patient can make, which in this case is whether to pursue reirradiation.6 The circle nodes represent the “states of nature” that are of interest, namely control or no control of the tumor after treatment and the presence or absence of grade 3 or higher toxicity. The probabilities for tumor control (defined as locoregional control) and symptoms (defined here as ≥ grade 3 toxicity) are adopted from the only randomized trial on postoperative head and neck reirradiation by Janot et al.4 Probability of control is 60% with treatment and 20% without treatment, with 30% chance of symptoms in the treatment branch and 10% in the no treatment branch.
Conditional probabilities are then constructed for each of the 4 possibilities for each branch based on the aforementioned probabilities:
- The probability of symptoms given control P(Symptoms|Control
- The probability of no symptoms given control P(¬Symptoms|Control)
- The probability of symptoms given no control P(Symptoms|¬Control)
- The probability of no symptoms given no control P(¬Symptoms|¬Control)
The patient will then assign their subjective values in the “Patient-Assigned Values” portion of the website for the 4 above conditional properties.
We have set the default parameters of “Control and No Symptoms” to 100 and “No Control and Symptoms” to 0, as this reflects the natural desire of most patients (these can be adjusted as well by the patient and/or oncologist). The patient will then fill out their values for “Control and Symptoms” and “No Control and No Symptoms” based on their individual risk tolerance. Once the values are set, the decision tree will calculate the expected values for the decision nodes (treatment or no treatment) by summing the product of all outcome values times their probabilities from right to left until we reach the decision node. The website will then highlight either the “Treat” or “No Treat” branch to show which choice should be preferred based on the entered information.
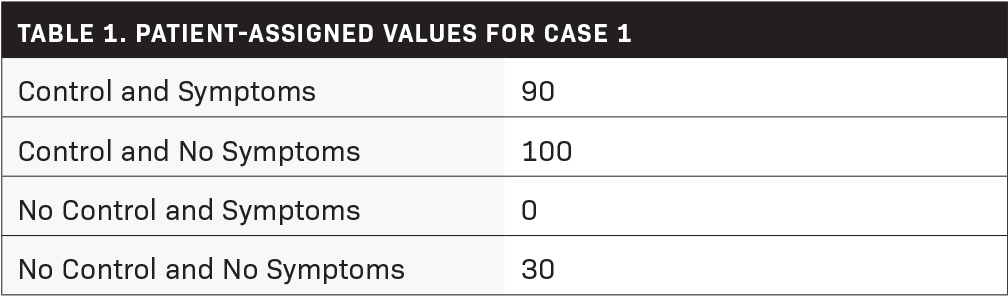
Case 1
A 65-year-old man with a history of a stage III (cT3N0M0) supraglottic squamous cell carcinoma completed chemoradiation to a total dose of 70 Gy in 35 fractions with cisplatin. The patient was found to have a local recurrence 2 years later and underwent a salvage laryngectomy where final pathology showed a rpT1N1M0 tumor with a close margin, as well as lymphovascular invasion. The patient wished to be aggressive, thus his preferences could be assigned values as shown in Table 1.
Entering these values into the decision tree, the expected utility for treatment was greater (Figure 1). This patient went on to receive postoperative reirradiation to a total dose of 60 Gy in 30 fractions.
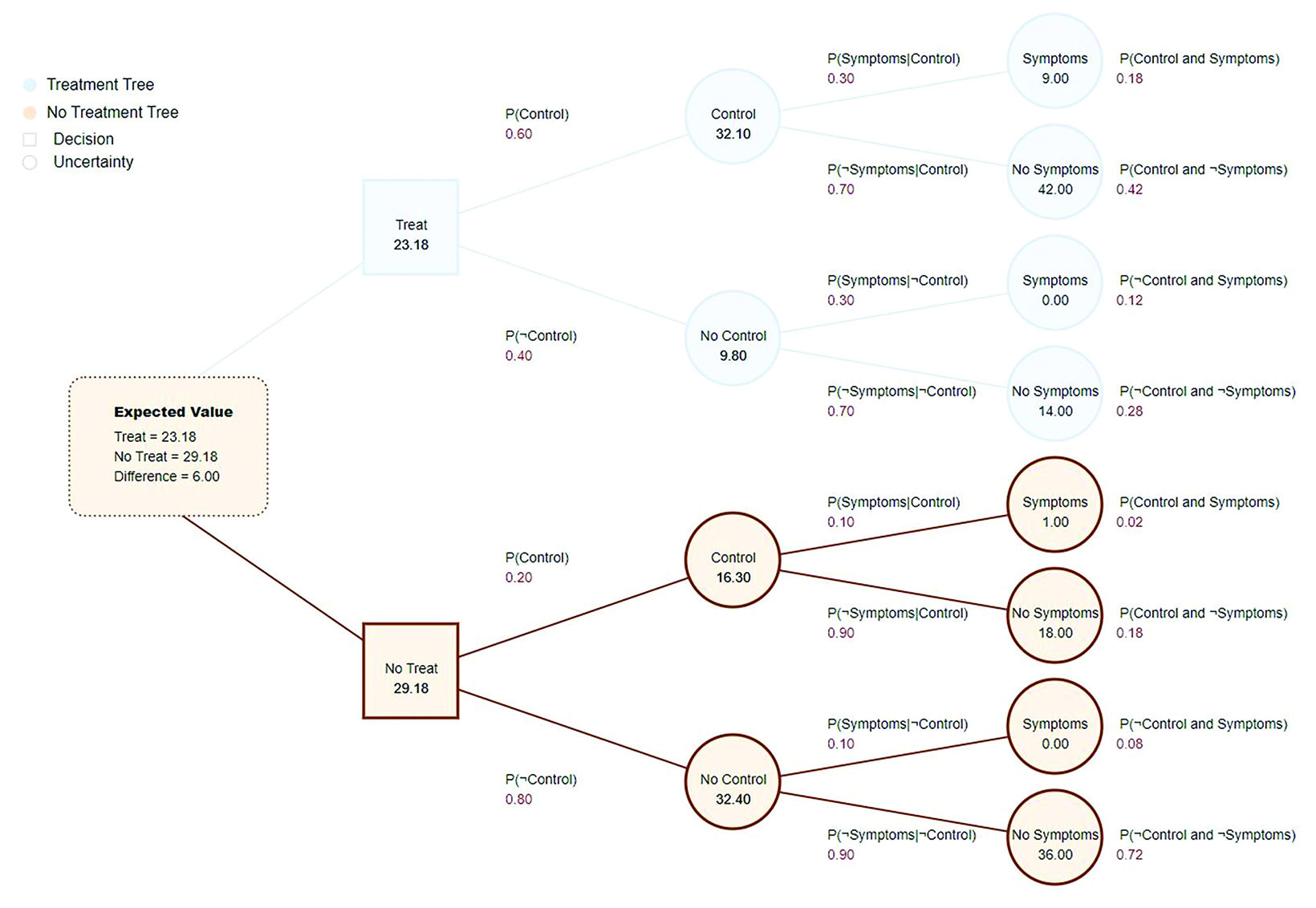
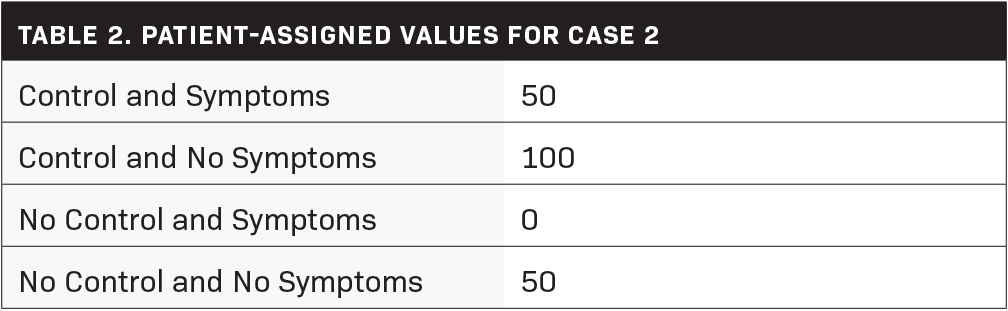
Case 2
A 46-year-old woman with a stage IVA (cT2N2aM0) left pyriform sinus supraglottic squamous cell carcinoma completed chemoradiation with cisplatin to a total dose of 70 Gy in 35 fractions. One year later, the patient experienced an in-field nodal relapse and underwent a salvage right modified radical neck dissection where she was found to have 7 out of 12 lymph nodes positive without evidence of extranodal extension. Reviewing treatment options with the patient, she was willing to consider a good outcome if there were minimal symptoms. Her treatment preferences could be modeled as shown in Table 2.
The expected utility favors observation in this scenario (Figure 2). This patient ultimately elected to undergo observation.
Discussion
These examples show how decision trees can aid our patients in making difficult decisions regarding reirradiation. The physician bears the responsibility of entering in the probabilities they feel best represent the choice between local control and morbidity from treatment. The probabilities can be adjusted; it was the author’s preference to use randomized control data, but others may wish to use other data and can change the probabilities from their analysis of the literature. The “Patient-Assigned Values,” however, should come from the patient’s themselves and will vary per individual. They can be entered and adjusted in real time on any web browser. This is a powerful and well-established way of decision making. In fact, McNeil, Weicheselbaum, and Pauker published an article in 1981 in the New England Journal of Medicine where they used expected utility theory (EUT) to discuss “decisions involving tradeoffs between quantity and quality of life” for patients with laryngeal cancer deciding between radiation therapy and surgery.9 Decision trees were also used by Plante et al (1987) to model various decisions that incorporated radiation and morbidity in treatment of pyriform sinus carcinoma.10 These papers were highly technical and difficult to use in real life. Now in the 21st century, using our web-based model, a patient can easily put in their preferences at any doctor’s visit for practical use of the decision tree. This powerful tool that was once hidden by technical jargon can now be utilized by all during a consultation.
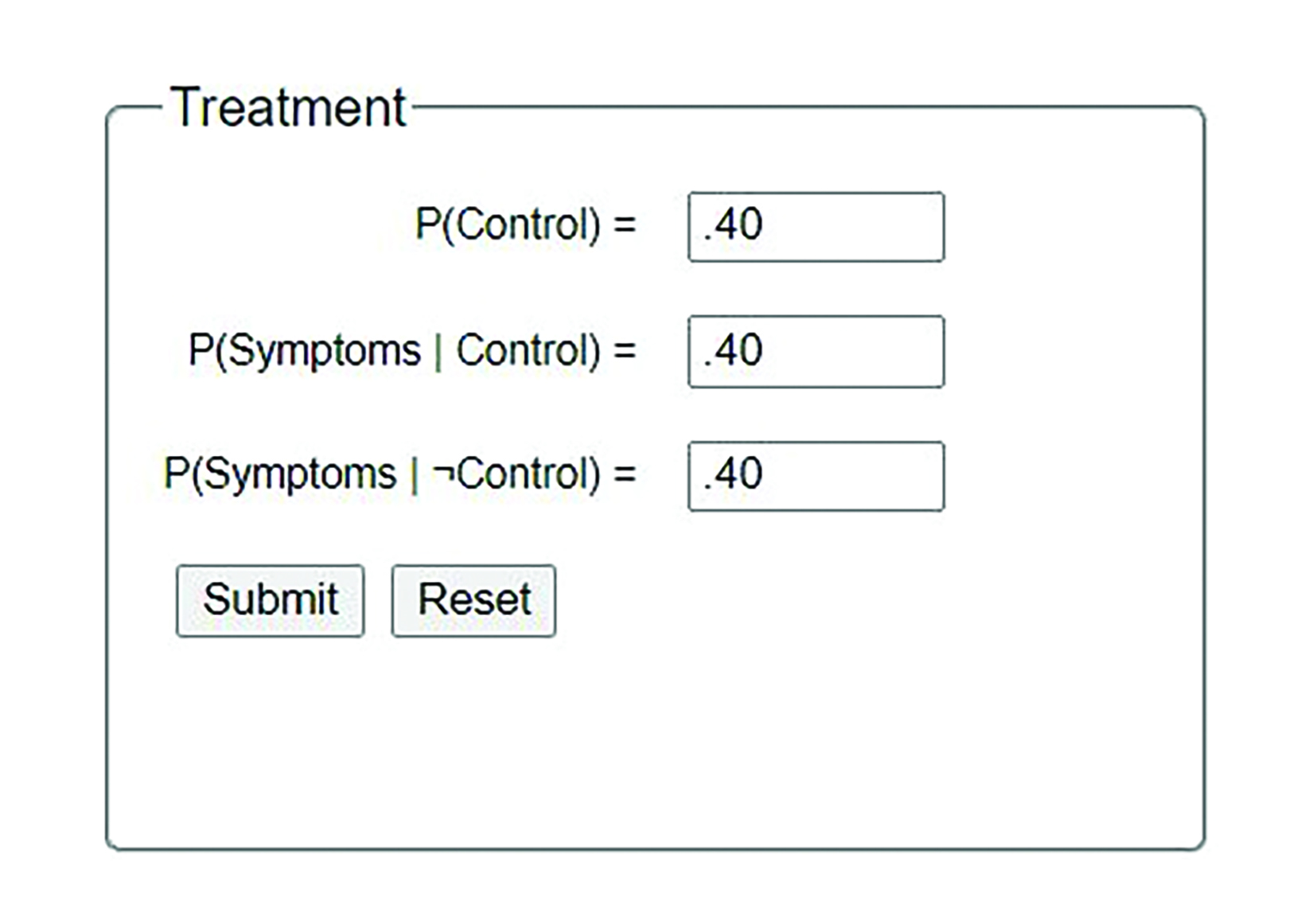
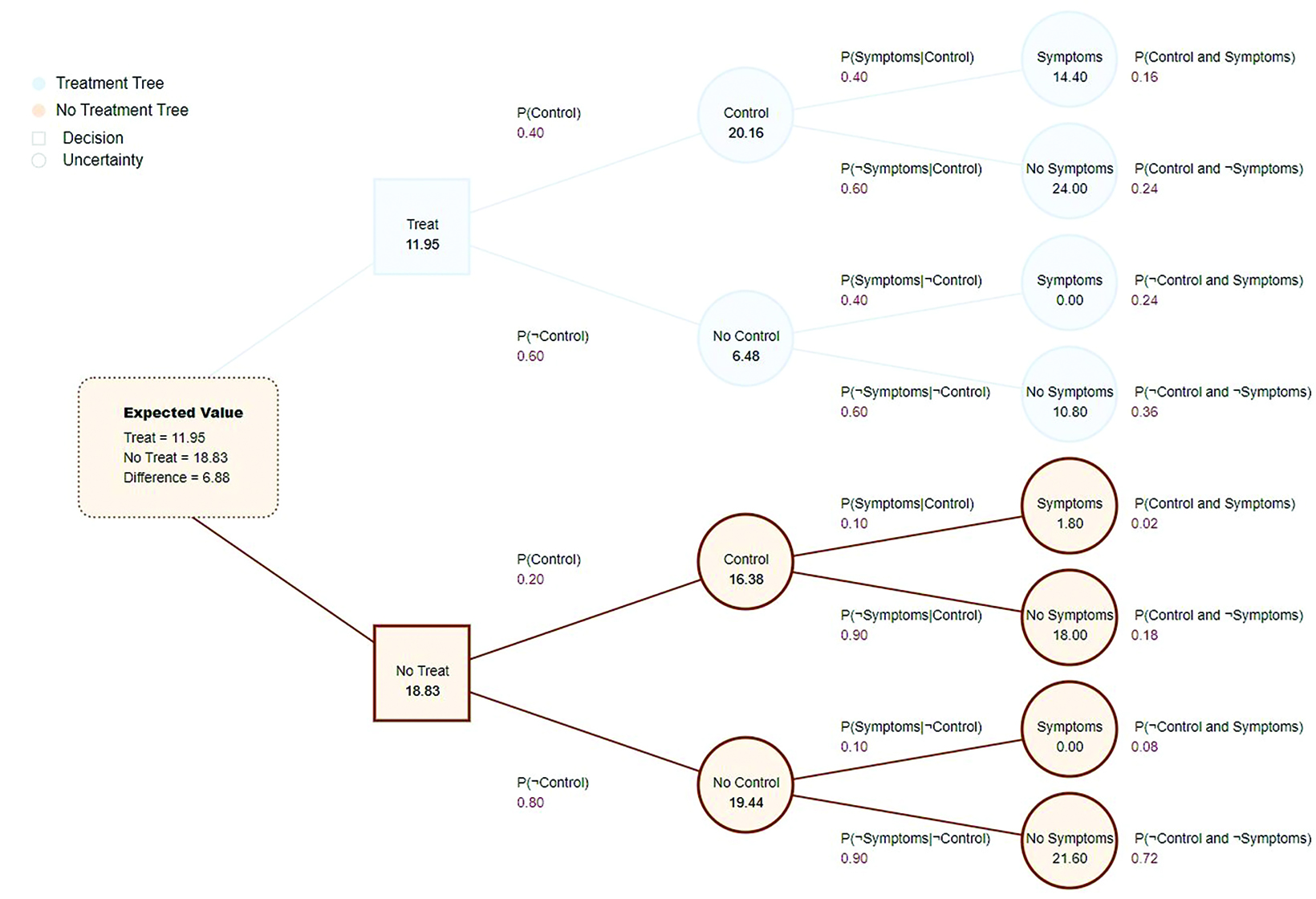
The authors recognize the limitations of EUT and the decision tree. EUT requires the Von Neumann-Morgenstern (VM) utility, which is more restrictive than the ordinal utility functions economists use for consumer theory. Ordinal utility only requires rank ordering of choices, whereas VM utility uses cardinal utility and relies on the patient knowing their strength of preference, which can be difficult. There is also vast literature debating the merits of expected utility, with common criticism related to loss aversion, ambiguity aversion, and decision-making with unawareness of all outcomes.7,11 Wu in his editorial “Strengths and Limitations of Expected Utility Theory” aptly cautions against abandoning EUT, “finding a utility model that includes the relevant psychological considerations, is developed from axioms that are reasonable guides for choosing among the appropriate medical alternatives, and can be assimilated into clinical practice.”12 Furthermore, in the current configuration, the decision tree only addresses the scenario of reirradiation after salvage surgery, but in theory could be adjusted for other scenarios (eg, reirradiation of recurrent tumor without surgery). Also, in an area with only 1 randomized trial and research mostly consisting of retrospective data, the probability estimates may be inaccurate. If one wishes to use other smaller prospective studies, such as the Dutch study, or incorporate data from studies that combined systemic therapy, or even SBRT reirradiation studies, one is free to do so.13-15 For example, we could use data from the 2018, phase II, European trial for reirradiation after salvage surgery that randomized once-daily split-course radiation therapy with concomitant chemotherapy or twice daily (BID) radiation therapy with cetuximab.14 The conclusion of the trial was favorable toward the BID cetuximab arm. If we used this regimen, we could simply change the numbers in the “Treatment” box on the website with the study’s data (Figure 3). Recomputing the decision for case 1 and assuming the no control arm would be the same, the expected utility for no treatment would be higher in this instance (Figure 4). Again, the physician can change these numbers easily on the website should newer data become available.
Conclusion
There are areas in medicine where data are not perfect and balancing uncertainty and patient preferences is paramount. Reirradiation after surgery is one of those areas and we must not forget to incorporate patient preferences when making these difficult decisions. The decision tree developed here is felt to be a reasonable guide to help both physicians and patients using all available background information. EUT and decision trees incorporate the oncologist’s knowledge of the data with the preference of the patient to help make the best personalized decisions. This web-based decision tree model is a practical and easy-to-access solution that will be useful in guiding those faced with the difficult decision of postoperative reirradiation in head and neck cancers.
References
- Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer Statistics, 2021. CA: Cancer J Clin. 2021;71(1):7-33. doi:10.3322/caac.21654
- McSpadden R, Zender C, Eskander A. AHNS series: Do you know your guidelines? Guideline recommendations for recurrent and persistent head and neck cancer after primary treatment. Head Neck. 2019;41(1):7-15. doi:10.1002/hed.25443
- Matoscevic K, Graf N, Pezier TF, Huber GF. Success of salvage treatment: a critical appraisal of salvage rates for different subsites of HNSCC.
- Otolaryngol Head Neck Surg. 2014;151(3):454-461. doi:10.1177/0194599814535183
- Janot F, de Raucourt D, Benhamou E, et al. Randomized trial of postoperative reirradiation combined with chemotherapy after salvage sur- gery compared with salvage surgery alone in head and neck carcinoma. J Clin Oncol. 2008;26(34):5518-5523. doi:10.1200/JCO.2007.15.0102
- North DW. A Tutorial introduction to decision theory. IEEE Transactions on Systems Science and Cybernetics. 1968;4(3):200-210. doi:10.1109/ TSSC.1968.300114
- Arsham H. Tools for Decision Analysis. Accessed November 26, 2021. http://home.ubalt.edu/ntsbarsh/business-stat/opre/partIX. htm#rtreeinflunce
- Steele K, Stefánsson HO. Decision Theory. In: Zalta EN, ed. The Stanford Encyclopedia of Philosophy. Winter 2020. Metaphysics Research Lab, Stanford University; 2020. Accessed November 20, 2021. https://plato.stanford.edu/archives/win2020/entries/decision-theory/
- Autor D. Lecture Note 14: Uncertainty, Expected Utility Theory and the Market for Risk. Accessed November 20, 2021. https://dspace.mit.edu/ bitstream/handle/1721.1/109484/14-03-fall-2010/contents/lecture-notes/MIT14_03F10_lec14.pdf.
- McNeil BJ, Weichselbaum R, Pauker SG. Speech and survival: tradeoffs between quality and quantity of life in laryngeal cancer. N Engl J Med. 1981;305(17):982-987. doi:10.1056/NEJM198110223051704
- Plante DA, Piccirillo JF, Sofferman RA. Decision analysis of treatment options in pyriform sinus carcinoma. Med Decis Making. 1987;7(2):74- 83. doi:10.1177/0272989X8700700203
- Dixit, AK. Notes for Lecture 10: Critiques of Expected Utility Theory. Accessed November 26, 2021. https://www.princeton.edu/dixitak/Teaching/EconomicsOfUncertainty/Slides&Notes/Notes10.pdf
- Wu G. The strengths and limitations of expected utility theory. Med Decis Making. 1996;16(1):9-10; discussion 14. Accessed November 26, 2021. https:// journals.sagepub.com/doi/abs/10.1177/0272989X9601600104
- Kasperts N, Slotman BJ, Leemans CR, de Bree R, Doornaert P, Langendijk JA. Results of postoperative reirradiation for recurrent or second primary head and neck carcinoma. Cancer. 2006;106(7):1536-1547. doi:10.1002/cncr.21768
- Tao Y, Faivre L, Laprie A, et al. Randomized trial comparing two methods of re-irradiation after salvage surgery in head and neck squamous cell carcinoma: once daily split-course radiotherapy with concomitant chemotherapy or twice daily radiotherapy with cetuximab. Radiother Oncol. 2018;128(3):467-471. doi:10.1016/j.radonc.2018.05.005
- De Crevoisier R, Domenge C, Wibault P, et al. Full dose reirradiation combined with chemotherapy after salvage surgery in head and neck carcinoma. Cancer. 2001;91(11):2071-2076. doi:10.1002/1097-0142(20010601)91:11<2071::aid-cncr1234>3.0.co;2-z
Citation
JH P, G G, T C. Utilization of Decision Theory and Decision Trees to Make Treatment Choices for Postoperative Reirradiation for Recurrent HNC. Appl Radiat Oncol. 2022;(2):35-39.
July 15, 2022