Pain flare and vertebral fracture following spine stereotactic radiosurgery for metastatic renal cell carcinoma
Images




Case Summary
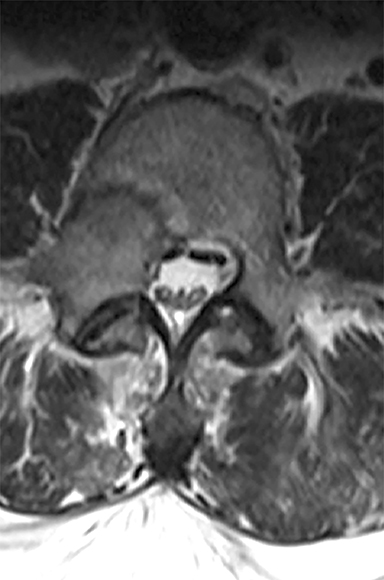
A 56-year-old man presented in December 2013 with lower extremity radicular pain, numbness and weakness. His medical history was significant for a pT3b renal cell carcinoma (RCC) diagnosed in January 2013 status post nephrectomy. At the time of consultation, physical exam demonstrated decreased sensation over the lateral aspect of his right leg. Two months prior, chest computed tomography (CT) had revealed several subcentimeter nodules suspicious for metastatic disease, and the patient was started on sunitinib. Due to concern for epidural disease, MRI of the lumbar spine was done, which revealed a destructive lesion within the L4 vertebra (Figure 1).
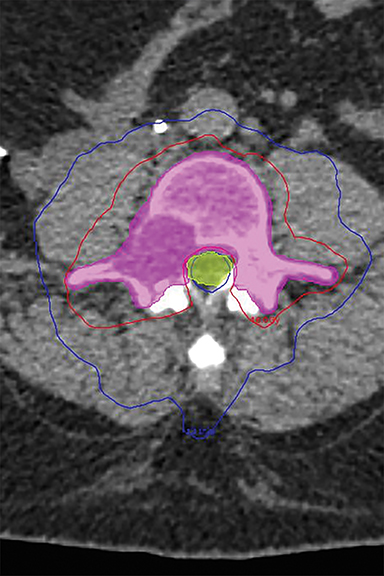
The patient met inclusion criteria for and was offered RTOG 0631, a phase II/III study of single-fraction stereotactic radiosurgery (SRS) vs. conventional external-beam radiation therapy (EBRT). The primary endpoint of this study is pain control. The patient was randomized to SRS and 16 Gy was prescribed to the L4 vertebral body and posterior elements (Figure 2). The cauda equina was constrained to V12 Gy ≤ 10% and maximum point dose < 16 Gy.
Shortly after completing SRS, the patient suffered from a pain flare at the treated site. A steroid taper was prescribed, and the pain rapidly resolved. Two weeks after SRS, the patient was seen in clinic and reported significantly decreased pain, resolved numbness, and increased strength.
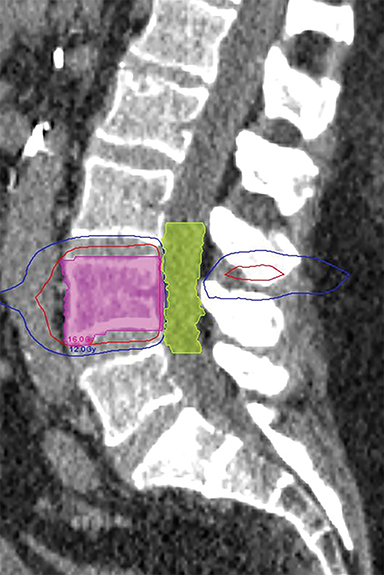
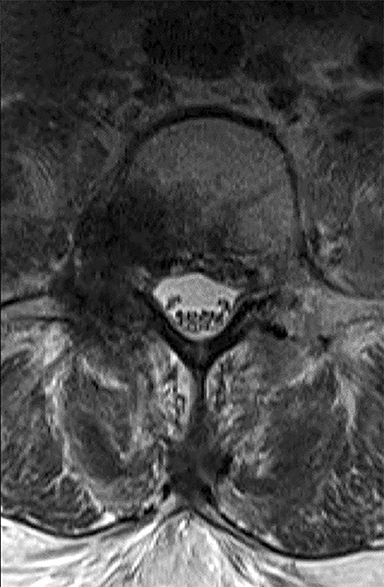
Six months after SRS, follow-up imaging demonstrated slight posterior wedging of the L4 vertebral body (Figure 3), and the decision was made to proceed with kyphoplasty. His systemic disease remained stable through May 2015, at which time an L2 metastasis was observed. The L4 metastases remains controlled through 25 months of follow-up (Figure 4).
Imaging Findings
Imaging of the lumbar spine at presentation demonstrated a 3.4-x-2.8-cm lesion within the right posterolateral aspect of the L4 vertebral body. This extended into the right pedicle, epidural space, and encroached upon the superior and inferior neural foramina (Figure 1).
After SRS, follow-up imaging in June 2014 demonstrated slight posterior wedging of the L4 vertebral body (Figure 3). Despite kyphoplasty, progressive asymptomatic height loss was observed throughout radiographic follow-up (Figure 4).
Discussion
This report demonstrates several areas of interest in the field of stereotactic radiosurgery of the spine. The incidence, time course, and risk factors for pain flare and vertebral compression fracture have been well-studied in multi-institutional and prospective investigations.1,2 In contrast, the use of targeted therapies with SRS has not been investigated in controlled settings, with conflicting evidence on safety and efficacy.3–5 While many retrospective and single-arm prospective investigations have suggested increased durability of symptomatic and radiographic control, results from RTOG 0631 are awaited to determine the relative benefit of SRS over EBRT.
Pain flare is a common and transient complication after radiotherapy to the spine. This complication arises within 2 weeks of treatment and is thought to occur secondary to ablation of neoplastic tissue and its associated bony instability. In general, however, these flares subside quickly and are generally amenable to a steroid taper.6 A 2013 prospective observational study of 41 patients undergoing hypofractionated SRS (24-35 Gy / 2-5 fractions) reported a 68% incidence of pain flare.2 Accordingly, select institutions have chosen to administer prophylactic steroids to all patients undergoing SRS.7 This practice is supported by a recent double-blind randomized trial that reported a decreased incidence of pain flare among patients administered prophylactic steroids undergoing palliative radiotherapy.8 In contrast, other investigations have reported modest rates of pain flare (15%) in the absence of prophylactic steroids, likely secondary to differences in prescription dose.6,9 Given the relatively low incidence of pain flare noted in our institutional series, we do not routinely treat patients undergoing spine SRS with prophylactic steroids.
Vertebral compression fracture is the most common late toxicity following SRS. While SRS and EBRT offer palliation of tumor-related discomfort, pain secondary to bony instability cannot be treated with radiation therapy, but may be alleviated with vertebral augmentation.10 In a multi-institutional study of 410 spinal segments treated with SRS, the 12-month cumulative incidence of fracture was 12%.1 A dose-response relationship was identified, with doses > 20 Gy per fraction associated with an increased risk for fracture. Because these fractures may lead to chronic mechanical pain, spinal segments may be reliably risk-stratified using the Spinal Instability Neoplastic Score.11 In high-risk cases, dose reduction may be appropriate in an effort to maximize patient quality of life.
Finally, an area of particular interest is the use of high-dose, hypofractionated radiation therapy with concurrent targeted therapies. Preclinical models have supported a synergistic relationship between angiogenesis inhibition and radiation, and uncontrolled retrospective series have reported excellent local control with combined therapy.5 Furthermore, the immunogenic characteristics of hypofractionated radiation therapy have been hypothesized to augment targeted immunotherapies.12 In the present report, a patient with oligometastatic renal cell carcinoma undergoing concurrent systemic therapy with an anti-angiogenic tyrosine kinase inhibitor (TKI) was treated with SRS. For patients undergoing upper thoracic or cervical SRS with concurrent TKIs, esophageal toxicity may be a significant concern.3 In addition, it is unknown whether rates of pain flare or fracture are increased with the use of combined therapy. Despite these concerns for safety, retrospective evidence has suggested a significant local control benefit with the addition of TKIs to SRS. In support of this hypothesis, local control has been durable through 25 months of radiographic follow-up in this patient. This efficacy may support a role for upfront aggressive treatment of oligometastatic disease with definitive intent. To explore this role, an ongoing cooperative trial (NRG-BR001) is investigating the safety of stereotactic body radiation therapy for oligometastatic disease.
Conclusion
This report demonstrates several key considerations associated with the use of spine stereotactic radiosurgery. Pain flare and vertebral compression fracture are common complications, which may be managed with steroids and vertebral augmentation. However, sequelae of tumor ablation may be irreversible, and fracture progression may lead to chronic mechanical pain. Despite this, SRS appears to achieve high rates of symptomatic and radiographic control, with limited data available describing the efficacy of SRS combined with targeted therapies.
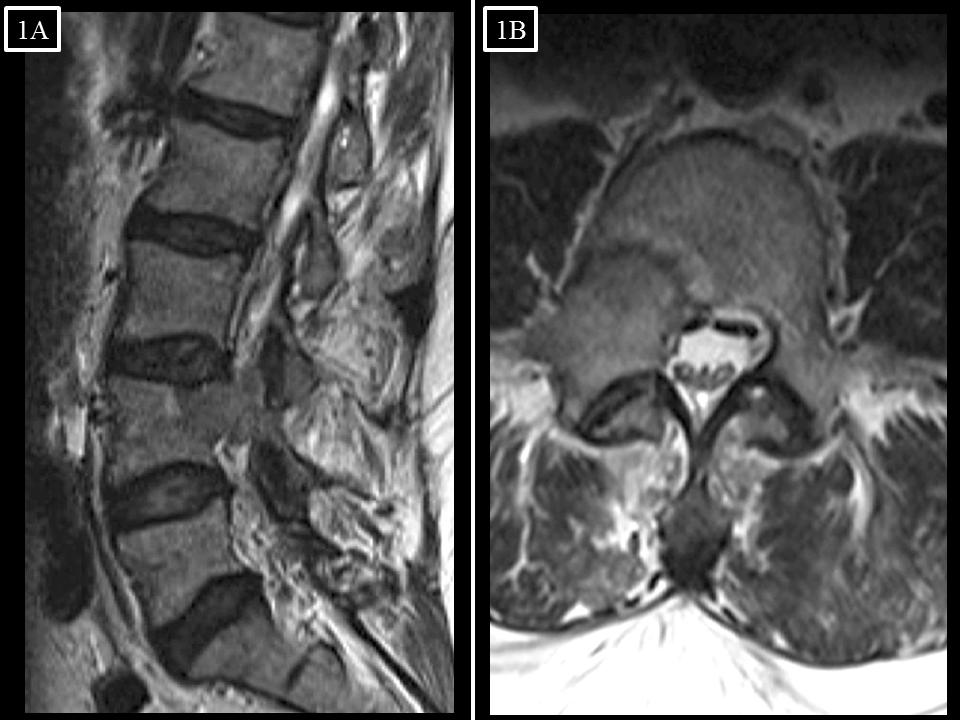
FIGURE 1. (A) Sagittal and (B) axial T2-weighted MR images of the lumbar spine upon presentation (12/2013) with lower extremity radicular symptoms. A lesion is present within the right posterolateral aspect of the L4 vertebral body, extending through the right pedicle and into the epidural space without effacement of the cauda equina.
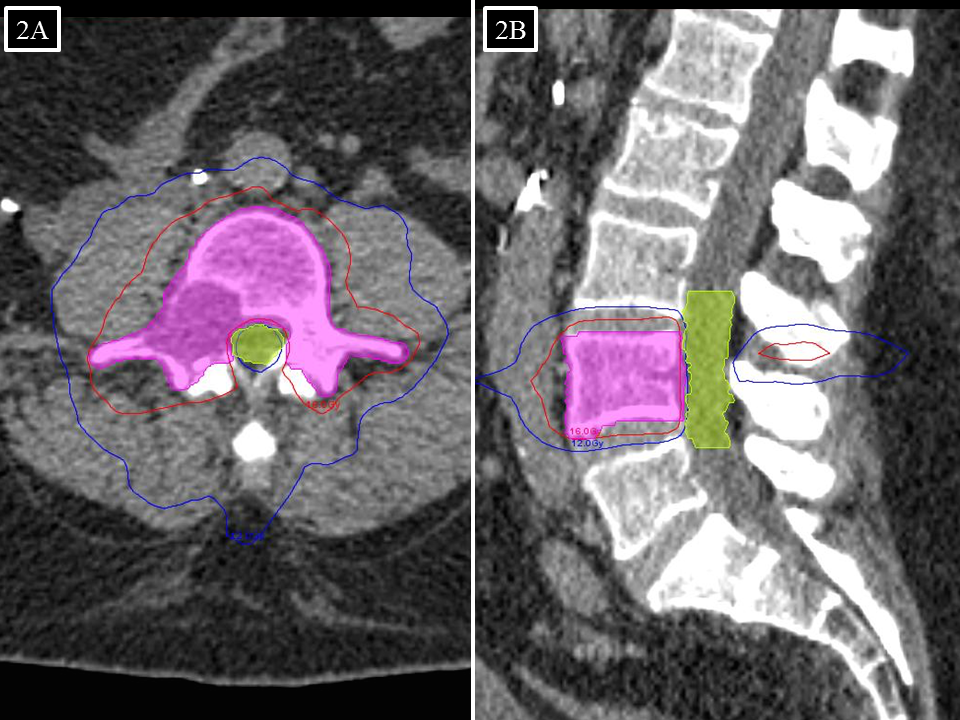
FIGURE 2. (A) Sagittal and (B) axial images of stereotactic radiosurgery plan for L4 vertebra, with 10 Gy (blue) and 16 Gy (red) isodose lines.
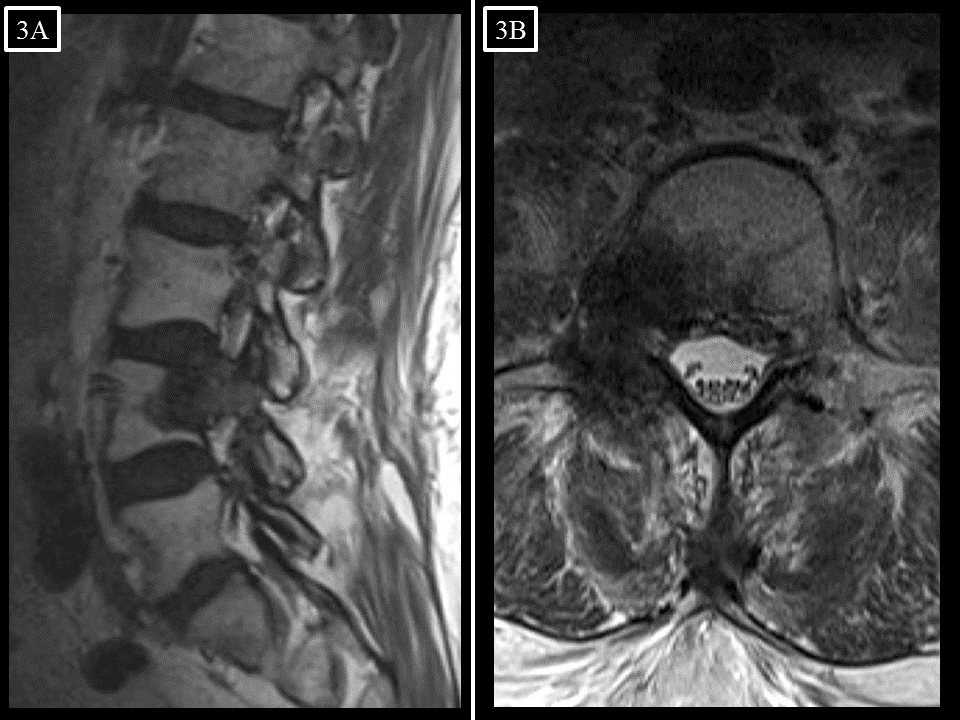
FIGURE 3. (A) Sagittal and (B) axial T2-weighted MR images of the lumbar spine 6 months following SRS (6/2014). The volume of epidural disease has decreased, and there is no evidence of local progression. However, this is slight posterior wedging of the L4 vertebral body.
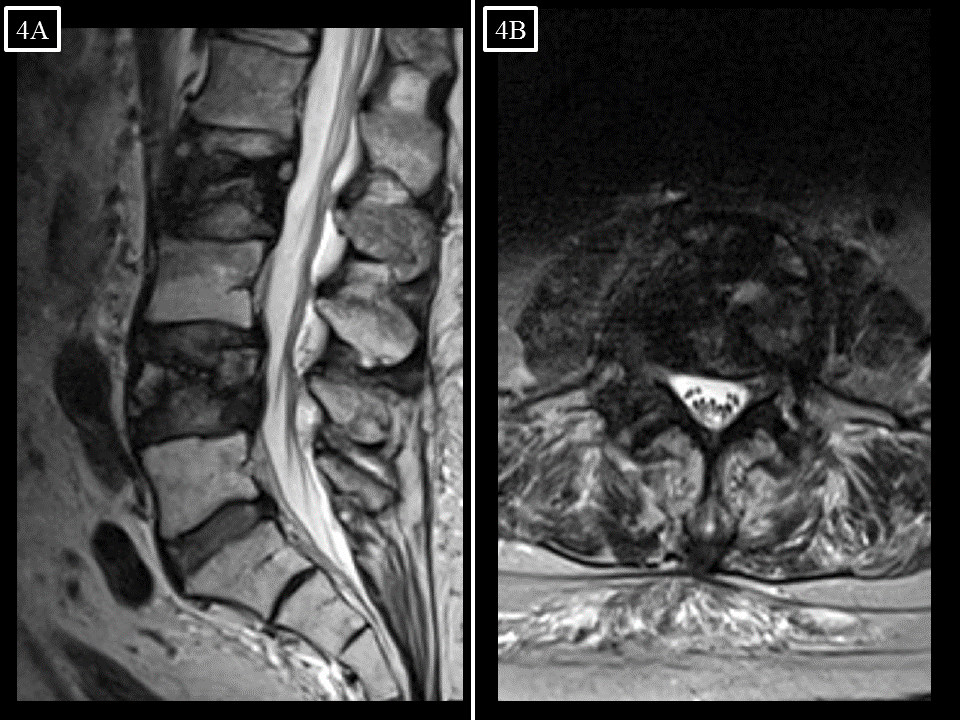
FIGURE 4. (A) Sagittal and (B) axial T2-weighted MR images of the lumbar spine 25 months following SRS (2/2016). There has been significant interval collapse of the L4 vertebral body without local progression, and an L2 metastasis is evident.
References
1. Sahgal A, Atenafu EG, Chao S, et al. Vertebral compression fracture after spine stereotactic body radiotherapy: a multi-institutional analysis with a focus on radiation dose and the spinal instability neoplastic score. J Clin Oncol Off J Am Soc Clin Oncol. 2013;31(27):3426-3431. doi:10.1200/JCO.2013.50.1411.
2. Chiang A, Zeng L, Zhang L, et al. Pain flare is a common adverse event in steroid-naïve patients after spine stereotactic body radiation therapy: a prospective clinical trial. Int J Radiat Oncol Biol Phys. 2013;86(4):638-642. doi:10.1016/j.ijrobp.2013.03.022.
3. Pollom EL, Deng L, Pai RK, et al. Gastrointestinal Toxicities With Combined Antiangiogenic and Stereotactic Body Radiation Therapy. Int J Radiat Oncol Biol Phys. 2015;92(3):568-576. doi:10.1016/j.ijrobp.2015.02.016.
4. Kao J, Chen C-T, Tong CCL, et al. Concurrent sunitinib and stereotactic body radiotherapy for patients with oligometastases: final report of a prospective clinical trial. Target Oncol. 2014;9(2):145-153. doi:10.1007/s11523-013-0280-y.
5. Staehler M, Haseke N, Nuhn P, et al. Simultaneous anti-angiogenic therapy and single-fraction radiosurgery in clinically relevant metastases from renal cell carcinoma. BJU Int. 2011;108(5):673-678. doi:10.1111/j.1464-410X.2010.09895.x.
6. Jung DL, Balagamwala EH, Angelov L, et al. Incidence and Risk Factors for Pain Flare Following Spine Radiosurgery. Int J Radiat Oncol Biol Phys. 2013;87(2):S568-S569. doi:10.1016/j.ijrobp.2013.06.1508.
7. Khan L, Chiang A, Zhang L, et al. Prophylactic dexamethasone effectively reduces the incidence of pain flare following spine stereotactic body radiotherapy (SBRT): a prospective observational study. Support Care Cancer Off J Multinatl Assoc Support Care Cancer. March 2015. doi:10.1007/s00520-015-2659-z.
8. Chow E, Meyer RM, Ding K, et al. Dexamethasone in the prophylaxis of radiation-induced pain flare after palliative radiotherapy for bone metastases: a double-blind, randomised placebo-controlled, phase 3 trial. Lancet Oncol. 2015;16(15):1463-1472. doi:10.1016/S1470-2045(15)00199-0.
9. Pan HY, Allen PK, Wang XS, et al. Incidence and predictive factors of pain flare after spine stereotactic body radiation therapy: secondary analysis of phase 1/2 trials. Int J Radiat Oncol Biol Phys. 2014;90(4):870-876. doi:10.1016/j.ijrobp.2014.07.037.
10. Gerszten PC, Germanwala A, Burton SA, Welch WC, Ozhasoglu C, Vogel WJ. Combination kyphoplasty and spinal radiosurgery: a new treatment paradigm for pathological fractures. J Neurosurg Spine. 2005;3(4):296-301. doi:10.3171/spi.2005.3.4.0296.
11. Fourney DR, Frangou EM, Ryken TC, et al. Spinal instability neoplastic score: an analysis of reliability and validity from the spine oncology study group. J Clin Oncol Off J Am Soc Clin Oncol. 2011;29(22):3072-3077. doi:10.1200/JCO.2010.34.3897.
12. Seung SK, Curti BD, Crittenden M, et al. Phase 1 study of stereotactic body radiotherapy and interleukin-2--tumor and immunological responses. Sci Transl Med. 2012;4(137):137ra74. doi:10.1126/scitranslmed.3003649.
Mr. Miller is a medical student at the Cleveland Clinic Lerner College of Medicine of Case Western Reserve University, Cleveland, OH. Dr. Balagamwala is a resident physician in the Department of Radiation Oncology, Dr. Mohammadi is a staff physician in the Brain Tumor and Neuro-Oncology Center, Dr. Mekhail is a staff physician in the Department of Pain Management, Dr. Suh is chairman of the Department of Radiation Oncology, and Dr. Chao is a staff physician in the Department of Radiation Oncology, all at the Cleveland Clinic, Cleveland, OH.
Citation
JA M, EH B, A M, N M, JH S, ST C. Pain flare and vertebral fracture following spine stereotactic radiosurgery for metastatic renal cell carcinoma. Appl Radiat Oncol. 2016;(1):28-30.
February 8, 2016