Case ReportHead & Neck cancerPatient Safety
Whole-brain radiation therapy in pregnant patients with brain metastases: Risks of ionizing radiation exposure to the fetus
Images

CASE SUMMARY
A 38-year-old, right-handed female with a 15 pack-year smoking history presented at 11 weeks gestation with a 3-day history of “heaviness” and numbness in her right leg, especially posterior to her knee. Her previous obstetrical history was significant for 1 pregnancy, which was electively aborted. Initially, a presumed diagnosis of lumbar plexopathy was made. Three days later, she presented with a seizure described as whole-body rigidity with her left arm bent upwards at the elbow and right arm extended, in a fencing position, accompanied by tongue biting and left facial droop lasting approximately 5 minutes. During her hospital stay, imaging studies were obtained, revealing a lung mass, followed by bronchoscopy with fine-needle aspiration, with pathology revealing a diagnosis of non-small cell lung carcinoma (NSCLC).
IMAGING FINDINGS
MRI without contrast of the brain revealed a 1.7 × 1.3-cm nodular focus of heterogeneous high T2 signal with apparent internal cystic foci along the paramedian aspect of the falx in the left parietal lobe, a second smaller lesion in the left frontal lobe with a round focus of high T2 signal measuring 0.9 cm, and several small (< 5 mm) foci of abnormal fluid attenuated inversion recovery (FLAIR) signal seen along the posterior aspect of the right insula and right frontal pole.
CT scan of the chest without contrast revealed a 1.4 × 1.3-cm lobulated nodule in the medial and anterior aspect of the lingula compatible with a primary bronchogenic neoplasm and left hilar adenopathy.
MRI of the abdomen and pelvis was unremarkable for mass or lymphadenopathy.
DIAGNOSIS
The diagnosis of stage IV (M1b) moderately differentiated non-small cell lung carcinoma favor adenocarcinoma was made. No molecular diagnostics (e.g., EGFR, ALK, ROS-1) were available.
DISCUSSION
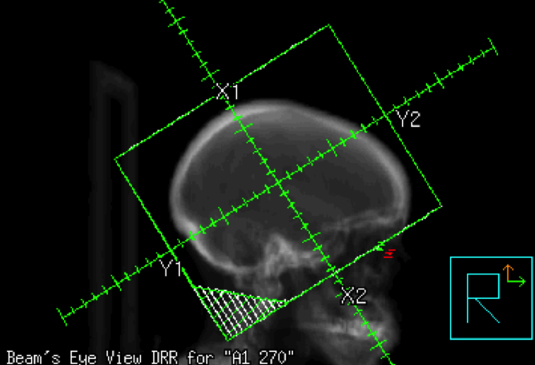
This case report presents a pregnant female seeking treatment for her newly diagnosed lung adenocarcinoma with brain metastases. The physician engaged in thoughtful discussion regarding the gravity of her diagnosis and the need for treatment, outlining various options including surgery, stereotactic radiosurgery (SRS), and whole-brain radiation (WBRT). Surgery was not considered as the patient had multiple brain metastases. A discussion was held on the benefit of SRS vs. WBRT. Given that SRS is associated with a higher risk of distant brain failure lending to a higher likelihood of retreatment during her pregnancy and the contraindication to administering gadolinium contrast, which further complicated accurate determination of the number of lesions and treatment targeting with SRS, WBRT alone was presented as the safest and most conservative management. The patient was also presented with the option of terminating her pregnancy to allow for more accurate staging, although termination was not a prerequisite to WBRT and subsequent systemic therapy. The patient expressed her desire for continuing her pregnancy unless doing so would jeopardize her life. The risks and benefits of WBRT were described in detail, including potential harms to the patient’s fetus. These included but were not limited to risks of mental retardation, organ malformations, and subsequent secondary malignancy in the child.1,2 Literature was referenced regarding case reports of healthy babies following head radiation. Magne et al highlighted a case of WBRT for a brain metastasis secondary to NSCLC, which exemplified the importance of discussing risks vs. benefits of therapy and respecting the patient’s desires regarding her pregnancy.3 In Magne’s case, the patient was faced twice with making the decision of accepting radiation therapy while pregnant or terminating the pregnancy. In the first instance she chose to terminate her pregnancy and sought radiation, while in the second she continued her pregnancy while receiving radiation therapy. Our patient continued her pregnancy and underwent WBRT at 14 weeks gestation to 3,750 cGy in 15 fractions with opposed lateral fields using 6MV photons. Figure 1 illustrates the fields used.
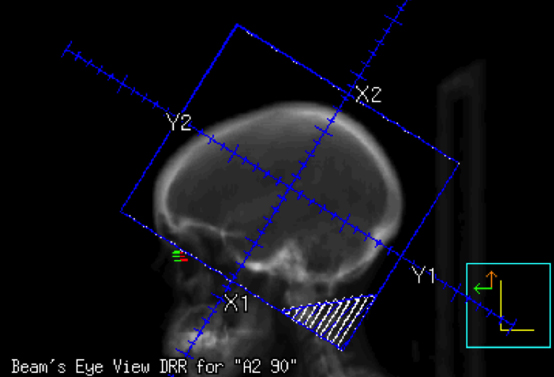
Report Number 50 of American Association of Physicists in Medicine (AAPM) Task Group 36 presents data and techniques to minimize radiation dose delivered to the fetus for radiation treatment delivered during pregnancy.1 In radiotherapy photon treatments, the dose outside the geometrical field size is caused by photons originating from either external scatter, which results from head leakage and scattering off high-Z materials used for the collimation system and beam modifiers, or internal scatter. Sneed et al has reported that 0.04% to 0.09% of the target dose is received by the fetus when implementing opposed lateral fields and bicoronal wedged arc fields to treat intracranial tumors.4 Compared to external scatter, internal scatter is a lesser contributor of the dose received by the fetus. Sneed et al reported internal scatter contributes to 13% to 20% of total fetal dose. This is consistent with the AAPM’s report, which states that at distances > 30 cm from the field edge, external scatter from head leakage becomes the greatest contributor of fetal dose. Internal scatter remains an unavoidable contributor to the peripheral dose, however dose to the fetus originating from head leakage can be minimized by implementing shielding during treatment.1 In this case, a 2-inch thick lead plate, representing 3.4 half-value layers, was positioned above the patient’s abdomen as illustrated in Figure 2. Other considerations include using the smallest radiation field, minimizing the use of secondary blocking, and maximizing the use of the primary block in the inferior aspect of the field, which all together minimizes external scatter. Also, the lowest energy was used to minimize neutron contamination seen with higher-beam energies.
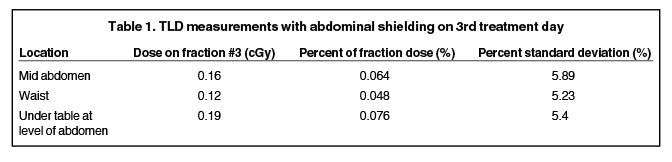
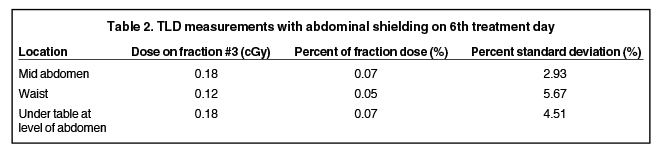
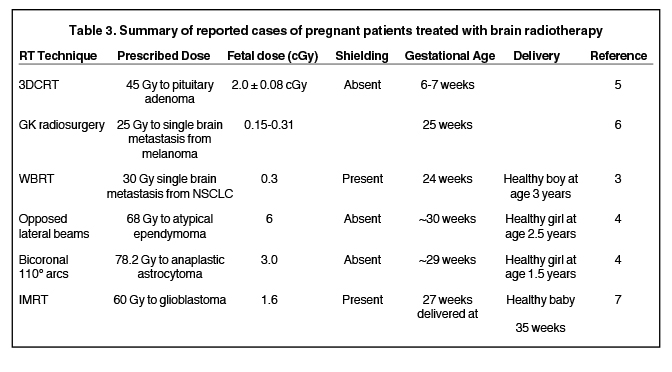
To approximate the dose delivered to the fetus, thermoluminescent dosimeter (TLD) measurements were obtained during radiation delivery with the abdominal shield in place. Nine TLDs were positioned, 3 each at the level of the midabdomen, waist, and under the table at the level of the abdomen. The average of the 3 TLD readings at each level was recorded for a given fraction. This data is summarized in Tables 1 and 2. AAPM Task Group 36 reported a small change in peripheral dose with depth ranging from 2 to 15 cm; therefore, average TLD measurements were used to extrapolate an estimated dose delivered to the fetus.1 The estimated fetal dose of 2.4 cGy (0.064% of target dose) is in keeping with previously reported data. Other reports of brain irradiation during pregnancy are summarized in Table 2, all of which remain below the generally accepted threshold of 10 cGy, above which fetal harm is associated.1
Upon completing radiation therapy, the patient met with her treating medical oncologist to consider systemic therapy. After discussing the risks and benefits of treatment she decided to accept adjuvant chemotherapy consisting of cisplatin and gemcitabine at 23 weeks gestation. The FDA has classified cisplatin and gemcitabine as pregnancy category D, yet reports have suggested that cisplatin and gemcitabine can be given without acute fetal toxicity, although no long-term follow-up exists for these children.8,9
The patient had a spontaneous rupture of membranes at 37 6/7 weeks gestation and vaginally delivered a healthy baby girl without complications. At last follow-up, marking 5 years following initial WBRT, the patient’s child had met all developmental milestones consistent with a healthy 5-year-old child. After initial therapy, the patient progressed to develop subsequent brain metastases, which were treated with Gamma Knife radiosurgery. The patient had no neurological sequelae from her disease.
CONCLUSION
In conclusion, we highlight a case of a 14-week pregnant female with newly diagnosed metastatic lung adenocarcinoma with brain metastases who was treated with WBRT and is now 5 years post therapy with a healthy 5-year-old girl. Our estimated cumulative fetal dose of 2.4 cGy delivered during treatment is consistent with data previously reported. We describe how with careful shielding, attempts can be made to reduce fetal dose to as low as is reasonably achievable. While a thorough discussion of the risks and benefits of any radiation exposure during pregnancy is vital prior to undergoing therapy, in our experience WBRT to a pregnant woman can be performed using techniques to minimize unnecessary radiation exposure to the fetus.
REFERENCES
- Stovall M, Blackwell CR, Cundiff J, et al. Fetal dose from radiotherapy with photon beams: report of AAPM Radiation Therapy Committee Task Group No. 36. Medical physics. Jan 1995;22(1):63-82.
- Wakeford R. Childhood leukaemia following medical diagnostic exposure to ionizing radiation in utero or after birth. Radiation protection dosimetry. 2008;132(2):166-174.
- Magne N, Marcie S, Pignol JP, Casagrande F, Lagrange JL. Radiotherapy for a solitary brain metastasis during pregnancy: a method for reducing fetal dose. The British Journal of Radiology. Jul 2001;74(883):638-641.
- Sneed PK, Albright NW, Wara WM, Prados MD, Wilson CB. Fetal dose estimates for radiotherapy of brain tumors during pregnancy. Int J Radiat Oncol Biol Phys. Jun 15 1995;32(3):823-830.
- Sharma DS, Jalali R, Tambe CM, Animesh, Deshpande DD. Effect of tertiary multileaf collimator (MLC) on foetal dose during three-dimensional conformal radiation therapy (3DCRT) of a brain tumour during pregnancy. Radiotherapy and oncology: Journal of the European Society for Therapeutic Radiology and Oncology. Jan 2004;70(1):49-54.
- Yu C, Jozsef G, Apuzzo ML, MacPherson DM, Petrovich Z. Fetal radiation doses for model C gamma knife radiosurgery. Neurosurgery. Mar 2003;52(3):687-693; discussion 693.
- Horowitz DP, Wang TJ, Wuu CS, et al. Fetal radiation monitoring and dose minimization during intensity modulated radiation therapy for glioblastoma in pregnancy. Journal of Neuro-oncology. Aug 6 2014.
- Wiesweg M, Aydin S, Koeninger A, et al. Administration of Gemcitabine for Metastatic Adenocarcinoma during Pregnancy: A Case Report and Review of the Literature. AJP Reports. May 2014;4(1):17-22.
- Dawood R, Instone M, Kehoe S. Neo-adjuvant chemotherapy for cervical cancer in pregnancy: a case report and literature review. European Journal of Obstetrics, Gynecology, and Reproductive Biology. Dec 2013;171(2):205-208.
