The trigeminocardiac reflex during linac- based hypofractionated stereotactic radiation therapy for a skull base tumor
Images
December 2016 Case Winner
CASE SUMMARY
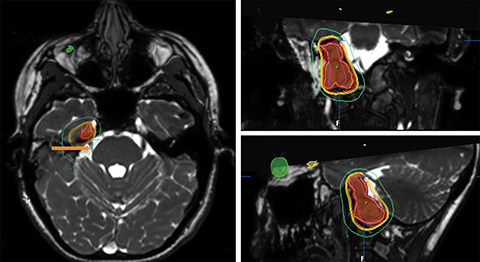
A 22-year old Caucasian woman presented with a recurrent right skull base paraganglioma after gross total resection. She underwent frameless linac-based hypofractionated stereotactic radiation therapy (FSRT) to 3000 cGy in 5 fractions (Figure 1). Three days after completing FSRT, the patient presented to the emergency department after experiencing syncope accompanied by diaphoresis, dizziness and nausea. Her blood pressure (BP) was 77/42 and heart rate (HR) 80 (baseline BP 110/75 and HR 110). She was given intravenous (IV) fluids and admitted for further management. Brain MRI showed no acute changes. During her 4-day hospitalization, she was managed with daily IV fluids and ondansetron. Her BP and HR normalized. Her symptoms improved throughout hospitalization and resolved by discharge. At 1-month follow-up, she remained healthy and denied further episodes.
IMAGING FINDINGS
No specific radiologic findings are associated with the trigeminocardiac reflex.
DIAGNOSIS
Trigeminocardiac reflex
DISCUSSION
The trigeminocardiac reflex (TCR) is clinically defined as the sudden onset of cardiac dysrhythmia, arterial hypotension, asystole, apnea, or gastric hypermotility.1 Although patients may not experience all of these autonomic symptoms, Schaller et al outlined that patients must have a > 20% decrease in mean arterial BP and HR from baseline for diagnosis of TCR.2 As a clinical diagnosis, there is no characteristic laboratory, radiologic, or pathologic findings associated with TCR. The TCR has been reported during orbit surgery, trans-sphenoidal surgery, cranio-maxillofacial surgery, and dermatologic surgery.1 The physiologic mechanism involves manipulation of the central or peripheral branches of the trigeminal nerve, Gasserian ganglion, or trigeminal brainstem centers and nuclei.1,3 The clinical manifestations are generally transient and resolve after removal of stimulus during surgery.1 However, the TCR has been associated with adverse outcomes in select cases, such as hearing loss or even death.4 Removing the mechanical stimulus on cranial nerve V during surgery generally immediately stops the reflex.5 This is widely considered the most important management step. If the reflex persists, based on a case report, Arasho et al suggest administration of IV atropine 0.6 mg (up to 2 doses) followed by 1 dose of IV epinephrine 6 μg if no response has been achieved.5 Several risk factors for TCR have been identified, such as age (more common in children), hypercapnia, hypoxemia, light anesthesia, narcotics such as sulfentanil, and preoperative beta-blockers or calcium-channel blockers.5 Careful identification and modification of risk factors should be considered. There may be a role for prophylaxis in cases with planned surgical manipulation near the trigeminal nerve. Mirakhur et al found that preoperative IV or intramuscular (IM) administration of 1 dose of either atropine (10-15 mg/kg) or glycopyrrolate (5-7.5 mg/kg) decreased the incidence of the oculocardiac reflex (OCR), a variant of the TCR, during ophthalmic surgery in children.6 Another study by Shende et al found decreased incidence and severity of OCR with local anesthetic blockade of the trigeminal nerve with bupivacaine.7
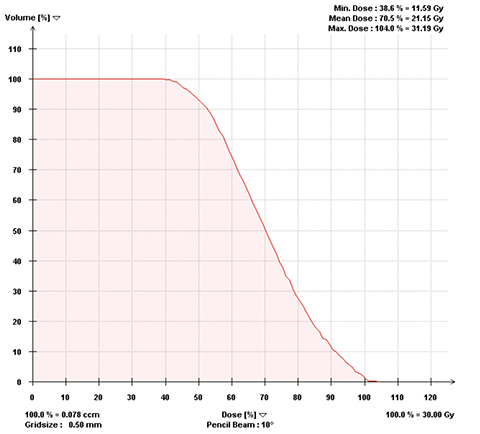
We believe that our patient’s clinical presentation is consistent with TCR. Her decrease in mean arterial BP and HR met the criteria discussed above. The onset of her symptoms was sudden. In addition, her nausea may have been related to gastric hypermotility. Given her tumor location, the trigeminal nerve and associated structures were within her RT treatment field (Figure 1). We have included the dose volume histogram for the trigeminal nerve (Figure 2) to demonstrate the dose received. Although her symptoms resolved with supportive care, the addition of a vagolytic agent may have been useful for management. Radiation-induced toxicity to the brainstem could partially explain her symptoms of nausea and dizziness, but would not cause the hemodynamic changes seen with our patient. Her previous skull base surgery may have caused scarring that predisposed her to chronic irritation of the trigeminal nerve. The patient was fairly young (age 22), but otherwise had no other previously identified risk factors. Additionally, there were no abnormal MRI findings to suggest another etiology.
Our case does differ from the classical presentation of TCR, as the patient’s symptoms manifested several days after completion of RT as a delayed TCR. Typically, the TCR presents during surgery with surgical manipulation of the trigeminal nerve. However, Chowdhury et al reported a case of delayed-onset TCR symptoms in a patient with an orbital floor fracture.8 The patient suffered from trauma causing a fracture of the orbital floor, and was managed conservatively. One month later, the patient developed a progressive and wide array of hemodynamic disturbances consistent with the TCR. A surgical procedure to correct the orbital fracture was performed and the patient’s cardiovascular symptoms improved dramatically. The authors concluded that was the first case of a chronic OCR.8 Compared to surgical manipulation, the intensity of stimulation on trigeminal nerve from radiation therapy (RT) in general is mild, sustained and accumulative.9 The biological consequences of exposure to ionizing radiation are mediated by a series of physical, chemical, biochemical, and cellular responses initiated after radiation is deposited in the tissue.10 This sustained stimulus on the trigeminal nerve and surrounding tissue occurs accumulatively during RT and persists even after RT completion.9 Thus, the intensity of RT stimulation may not be initially strong enough to induce the TCR symptoms. After a course of RT, the cumulative intensity of radiation stimulation could reach a threshold to induce TCR symptoms as observed in this case. Our atypical presentation of TCR associated with RT appears consistent with the findings reported by Chowdhury et al.8
CONCLUSION
We present a case of radiation-induced TCR in a patient with a skull base tumor treated with linac-based FSRT. The TCR has not been previously reported in association with RT. The clinical presentation of radiation-induced TCR described in this case differs from the classical intraoperative presentation, as it occurred several days after RT completion. We discussed the role of supportive care and vagolytics in managing radiation-induced TCR. Because TCR has been linked to adverse clinical outcomes, radiation oncologists should be aware of TCR as a potential phenomenon when treating patients with skull base tumors. Additional reports describing TCR during RT would certainly help further our understanding.
REFERENCES
- Schaller B. Trigeminocardiac reflex. A clinical phenomenon or a new physiological entity? J Neurol. 2004;251:658-665.
- Schaller B, Probst R, Strebel S, et al. Trigeminocardiac reflex during surgery in the cerebellopontine angle. J Neurosurg. 1999;90:215-220.
- Schaller B, Cornelius JF, Prabhakar H, et al. The trigemino-cardiac reflex: an update of the current knowledge. J Neurosurg Anesthesiol. 2009;21:187-195.
- Gharabaghi A, Koerbel A, Samii A, et al. The impact of hypotension due to the trigeminocardiac reflex on auditory function in vestibular schwannoma surgery. J Neurosurg. 2006;104:369-375.
- Arasho B, Sandu N, Spiriev T, et al. Management of the trigeminocardiac reflex: facts and own experience. Neurol India. 2009;57:375-380.
- Mirakhur RK, Jones CJ, Dundee JW, et al. I.m. or i.v. atropine or glycopyrrolate for the prevention of oculocardiac reflex in children undergoing squint surgery. Br J Anaesth. 1982;54:1059-1063.
- Shende D, Sadhasivam S, Madan R. Effects of peribulbar bupivacaine as an adjunct to general anaesthesia on peri-operative outcome following retinal detachment surgery. Anaesthesia. 2000;55:970-975.
- Chowdhury T, Cappellani RB, Schaller B. Chronic trigemino-cardiac reflex in patient with orbital floor fracture: role of surgery and first description. J Neurosurg Anesthesiol. 2014;26: 91-92.
- Mukherjee D, Coates PJ, Lorimore SA, et al. Responses to ionizing radiation mediated by inflammatory mechanisms. J Pathol. 2014;232: 289-299.
- Mitchell JB, Russo A, Kuppusamy P, Krishna MC. Radiation, radicals, and images. Ann N Y Acad Sci. 2000;899:28-43.
Citation
Roy A, Staecker H, Kumar P, Wang F. The trigeminocardiac reflex during linac- based hypofractionated stereotactic radiation therapy for a skull base tumor. Appl Rad Oncol. 2016;(4):42-44.
December 12, 2016
