Management of Head and Neck Cancer Patients During the Epidemic of COVID-19 in Wuhan
Images


SA-CME credits are available for this article here.
At the end of December 2019, an outbreak of the 2019 novel coronavirus disease (COVID-19) broke out in Wuhan, China.1 The virus has been identified as a novel β-coronavirus homologous to severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS) viruses.2 Current research demonstrates that the virus is mainly transmitted through respiratory droplets and direct contact. This virus has also been detected in saliva, feces, urine and other samples and, therefore, other routine methods of transmission cannot be excluded.3 The entire population is susceptible to this virus, for which the incubation period is relatively long (median incubation time 4 days) and the mortality rate from early retrospective studies in China is high (1.4% to 4.3%).4,5 On March 11, 2020, the World Health Organization (WHO) declared COVID-19 a pandemic. As of April 29, 2020, more than 3,000,000 confirmed cases have been reported in more than 200 countries and regions, resulting in over 207,000 deaths (https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200429-sitrep-100-covid-19.pdf?sfvrsn=bbfbf3d1_2). The epidemic continues to spread rapidly. The world is facing increasing pressure for epidemic prevention and control, and the medical system is already overloaded in many areas.
Soon after the epidemic broke out, strict prevention and control measures were adopted across China. Among them, Hubei, especially Wuhan City, where the epidemic was most severe, implemented unprecedented measures to lock down the city. All traffic in and out of Wuhan was suspended, including flights, trains, buses, boats, and private cars. All communities were strictly isolated and screened for infected patients. To cut the chain of transmission and to isolate all suspected and confirmed cases into confined treatment areas, the government converted a large number of hospitals into infectious disease prevention and treatment sites. Meanwhile, several large designated prevention and treatment hospitals for COVID-19 in Wuhan were quickly built while numerous medical staff were recruited to participate in the epidemic prevention and control work.
Under such circumstances, cancer patients face significant difficulties in disease diagnosis and treatment. First, cancer patients are often immunosuppressed due to the effects of cancer and anti-cancer treatment, and thus are prone to infection with the novel coronavirus. As a result, the prognosis after infection for cancer patients is worse than that of the general population.6 Second, under the rigid epidemic prevention measures, all cancer patients were also subject to strict restrictions similar to other local residents and were unable to start or continue their prescribed cancer treatment, or enter treatment facilities. Third, during isolation, the psychological pressure of patients increases sharply,7 along with nutrition and sleep disorders, all of which adversely impact treatment and recovery. Fourth, in order to stop the nosocomial spread of the epidemic, most of the cancer centers and oncology departments in Hubei Province, especially in Wuhan, ceased normal operation. Last but not least, many oncology medical staff were deployed to frontline anti-epidemic work, making it particularly difficult for cancer patients to obtain adequate cancer diagnosis and treatment.
Head and neck (HN) cancer is a common malignancy worldwide and is more prevalent in China. Radiation therapy and chemotherapy comprise the cornerstones of HN cancer treatment.8 For potentially curable tumors, early detection, diagnosis, and early treatment are critical to increase the cure rate and improve patient survival. However, during the COVID-19 epidemic, the diagnosis and treatment of HN cancer patients has been greatly affected. Strategies to maximally prevent viral infections and, at the same time, maintain adequate anti-tumor treatment are outstanding issues under consideration. Since the outbreak of COVID-19, the Cancer Institute of Zhongnan Hospital of Wuhan University has been in the center of the epidemic. We have therefore adopted a specific approach for cancer diagnosis and treatment during this period. This review summarizes diagnosis and treatment strategies for patients with HN cancer during the epidemic at our institute.
Inpatient Management
Management of Wards
In the early stages of the COVID-19 outbreak, given that hospitals are high-risk areas for the spread of disease and that cancer patients might be particularly vulnerable to viral infections, we discharged most cancer patients (who are typically inpatient for concurrent chemoradiation) home from the hospital according to the overall deployment plan of our local hospital. We instructed patients and their families to maintain close contact with our medical staff, with guidance on how to decide when to return to the hospital and continue cancer treatment. Nevertheless, a few patients failed to leave the hospital on time due to city lockdown and transport suspension. Since some were receiving radiation therapy and chemotherapy, we decided to continue with the treatments. Relying on the Law of the People’s Republic of China on the Prevention and Treatment of Infectious Diseases and Diagnosis and Treatment Protocol for Novel Coronavirus Pneumonia released by the National Health Commission and National Administration of Traditional Chinese Medicine, and the Institutional Guide of Coronavirus Infection Prevention and Control of Zhongnan Hospital of Wuhan University, we temporarily transformed the wards into a clean area, a potentially contaminated area, and a contaminated area. All medical staff including radiation oncologists, medical physicists, radiation therapists, nurses, and environmental services personnel underwent mandatory training on the prevention and control of the novel coronavirus. All personnel were required to strictly implement disinfection and wear personal protective equipment upon entering and leaving contaminated areas to protect the medical staff and prevent iatrogenic infections. For all patients remaining in the hospital, we designated individual rooms for each patient, and asked patients to follow guidelines and restrict their activities in the designated area. Patients with symptoms or suspected of viral infection were isolated and managed in the contaminated area. To reduce the risk of virus transmission, we asked patient family members to avoid unnecessary visits and our full-time nursing staff would distribute meals and take care of other daily activities.
Epidemic Surveillance
To closely monitor the epidemic, we adopted several strategies. First, we performed temperature monitoring twice daily for all medical staff and patients in the hospital. Patients presenting with suspected symptoms, such as fever, fatigue, cough, sputum, shortness of breath, myalgia, diarrhea and other symptoms, were immediately isolated and screened for novel coronavirus infection. These included routine blood tests, liver and kidney function, complete set of respiratory pathogens, influenza virus testing, procalcitonin (PCT), C-reactive protein (CRP), etc.9 Chest computed tomography (CT) was obtained in cases of suspected pneumonia. Later, when the detection of nucleic acid and antibodies of the novel coronavirus were available, both tests were performed to determine whether the patient was infected. Clinically suspected patients such as those with typical symptoms and atypical CT images but without positive viral detection were subjected to multidisciplinary consultations with experts from the Department of Infectious Diseases, the Department of Respiratory Medicine, and the Department of Critical Care Medicine. Any confirmed cases were transferred to the Department of Infectious Diseases for isolated treatment of COVID-19 during which period the anti-cancer treatment would be suspended. As of the date of report, there have been no confirmed cases of COVID-19 involving the medical staff nor a new infected case of COVID-19 among patients subsequently treated in our department.
Management of Radiation Therapy
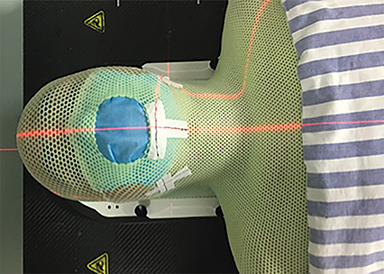
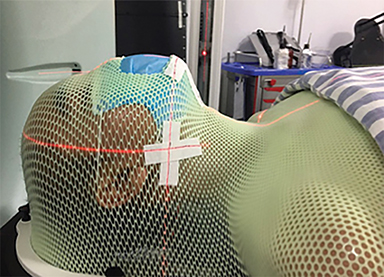
Radiation therapy is a key modality of cancer treatment. Given the unique property of accelerated repopulation of cancer cells after receiving radiation, radiation therapy should not be interrupted for any length of time during the treatment course.10 Since both infection prevention and cancer treatment greatly affect a patient’s survival and quality of life, a panel of experts agreed to maintain radiation therapy for patients requiring radiation treatment as a single modality. We set up temporal adapted treatment protocol and procedures, and reported to the hospital. Before all treatments, patients were fully informed about the risk of potential viral infection, and had to sign a Risk Notification of Novel Coronavirus Infection During Radiation Therapy prior to treatment, which emphasized the importance of the continuity of radiation therapy and the potential risk of infection. Patients were asked to strictly follow the guidance of radiation oncologists and obey the prevention and control measures during their treatment. Individual appointments were strictly implemented for simulation and each radiation therapy treatment, thereby minimizing waiting time. Sterilization and protective measures were applied for each patient at each step of treatment (Figure 1). Figure 1 shows a patient wearing a face mask under the conventional immobilization head mask. Patients were also asked to comply with appointment times to avoid crowds and infection. Radiation therapists were equipped with protective clothing, masks, and gloves and disinfectants (hand hygiene) (Figure 2) to reduce iatrogenic infections. As of the date of report, our center has collectively treated 48 HN cancer patients, of whom 46 completed radiation therapy, and 2 patients were still undergoing treatment. Among them, 3 patients with nasopharyngeal carcinoma successfully completed definitive concurrent chemoradiation therapy. Patients who completed their treatment were screened for COVID-19. No infections were detected and these patients were discharged. During the epidemic, around 30 patients (about 30%) in the HN Cancer Department had treatment delay (about two-and-a-half months) or interruption. Studies of the effect of radiation therapy delays or interruptions on cancer patients are ongoing.
Management of Chemotherapy
Cisplatin-based chemoradiation therapy is a necessary component of the standard of care for locally advanced HN cancer ineligible for surgery, or as part of adjuvant treatment.11 High-dose cisplatin can result in frequent severe adverse effects. To further minimize the side effects of concurrent chemoradiation therapy during the epidemic, we used alternative chemotherapy drugs with a lower toxicity profile. For example, studies in nasopharyngeal carcinoma showed that concurrent chemoradiation therapy with nedaplatin showed comparable effects to concurrent chemoradiation therapy with cisplatin, but significantly reduced gastrointestinal toxicity and ototoxicity. However, nedaplatin increases the risk of myelosuppression.12 Therefore, we delivered concurrent chemotherapy with nedaplatin to patients and strengthened supportive care for hematopoetic toxicity. Within 48 hours of chemotherapy completion, pegylated recombinant human granulocyte colony-stimulating factor (PEG-rhG-CSF) was administrated to reduce the risk of myelosuppression caused by chemoradiation. In monitoring myelosuppression, routine blood tests were performed at least twice a week and other supportive treatments such as erythropoietin and thrombopoietin were used in cases of severe anemia and thrombocytopenia, respectively. During the epidemic, patients tolerated the treatments well with no grade III-IV toxicities.
Supportive Treatments
During the outbreak, we also reinforced nutritional support for HN cancer patients. Oral hygiene, and radiodermatitis prevention and treatment were also carried out. Additionally, we offered psychological counseling for patients to mitigate their anxiety, fear and depression. We also encouraged patients to maintain communications with their family through video and telephone calls, and to report any discomfort during their hospital stay.
Outpatient Management
Epidemic Prevention and Education
We encouraged outpatients to remain in close contact with their doctor-in-charge and explained the real-time situations of epidemics and the possible influence on their disease and treatment. We tried to reduce patient anxiety regarding potential treatment delays and interruption. We also explained through telephone and social networks to patients and their families about the prevention and control of the epidemic. First, we advised that they should follow government guidelines, avoid going out and congregating in crowds, take body temperature daily, and report to the community epidemic prevention management agencies when pneumonia-like symptoms arose. Second, we advised that patients should wear masks, ensure frequent hand hygiene, and avoid direct contact with unknown persons. Thirdly, patients were encouraged to exercise regularly, ensure adequate sleep, maintain a positive mood, improve nutrition, etc. Fourth, should the patient or family members develop fever, cough, sputum, chest tightness, dyspnea, diarrhea and other symptoms, they were instructed to immediately report to their epidemic prevention management agency, check for viral infections, and accept isolated observation or treatment in case of confirmed infection, etc.
Medical Treatments
Chemotherapy for outpatients with HN cancer mainly includes induction chemotherapy, maintenance treatment for patients whose radiation therapy course was interrupted, and salvage chemotherapy for patients with relapsed or metastatic cancers. Due to the duration of traffic restrictions and personnel isolation during the epidemic, most patients could not undergo regular chemotherapy, and some patients who required radiation therapy could not start or complete ongoing radiation therapy. To ensure the continuity of cancer treatment and to prevent cancer progression, we recommended oral chemotherapy drugs under the guidance of medical oncologists to control tumor growth while reducing the incidence of viral infections during recurrent visits to the hospitals. Additionally, we also educated patients to be aware of potential adverse effects and how to manage these adverse effects.
For example, oral fluorouracil derivatives showed anti-cancer effect in nasopharyngeal carcinoma, and were well tolerated; most adverse effects were easily managed. Oral capecitabine showed good effects as neoadjuvant chemotherapy in locally advanced nasopharyngeal carcinoma, as single-agent chemotherapy in relapsed or metastatic nasopharyngeal carcinoma, and was superior as maintenance treatment vs observation in metastatic nasopharyngeal carcinoma.13-15 S-1 is another derivative of oral fluorouracil that also showed anti-cancer effect as concurrent chemoradiation therapy, or as salvage chemotherapy for relapsed or metastatic nasopharyngeal carcinoma.16-18 Common adverse effects of oral fluorouracil derivatives included fatigue, hand and foot syndrome, myelosuppression, nausea, vomiting, diarrhea, oral mucositis, and skin pigmentation. We required that doctors-in-charge maintain close contact with patients undergoing oral chemotherapy via phone or social network, and promptly guide patients to deal with possible side effects. When adverse effects occurred during treatment, the patients were asked to report to their doctor-in-charge who would evaluate the degree of the adverse effect and then guide symptomatic treatment. Treatments were discontinued in cases of severe adverse effects. For some patients with advanced HN cancers, appropriate nutritional support and analgesic treatment were recommended to their community doctors during the epidemic.
Catheter Maintenance
Some patients left the hospital with central venous catheters, mostly peripherally inserted central catheters (PICC). According to PICC nursing routines, patients were required to perform PICC maintenance at least once a week to reduce the occurrence of catheter-related complications such as catheter blockages, infections, and catheter-associated thrombi.19 Our institute maintained PICC clinics for patients in Wuhan who needed PICC maintenance. Individual appointments, screens for viral infection, adequate staffing, and patient protection measures were in place for the scheduled PICC maintenance. For patients residing outside Wuhan who found it difficult to come for scheduled PICC maintenance, considering that PICC might not be used for a long period, we recommended that PICC be removed at the nearest medical site.
Nutrition Education
During radiation therapy and chemotherapy, patients with HN cancer often suffer appetite loss and malnutrition due to adverse reactions including gastrointestinal side effects, xerostomia, and swallowing dysfunction. Therefore, nutrition education and, if necessary, nutrition interventions were addressed during the outbreak. Through communication among attending physicians, patients and their families, it was essential to follow the eating habits and the nutritional status of patients and to guide them to eat more protein-rich, digestible food, and balanced diets. We also encouraged patients to quit smoking and drinking alcohol. Appropriate enteral nutritional products could also be supplemented, according to their nutritional status. In case of malnutrition, regular blood tests and electrolytes analysis guided nutrition support treatment in the nearest medical site.
Psychological Interventions
Great psychological pressures arise in HN cancer patients and their families, which manifest as anxiety, nervousness, irritability, decreased appetite, and poor sleep quality, etc. The main sources of psychological stress for patients were uncertainty of the epidemic, anxiety about the interruption or delay of treatment, and fear of disease progression. In addition, long-term isolation and cancer-associated symptoms also increase the patient’s psychological pressure. In response to this situation, the attending physicians encouraged the patient to establish confidence via mutual communications, and make proper arrangements for treatments and management of adverse reactions during the epidemic. For some patients with greater psychological pressure, specific psychological interventions from professional psychologists and psychiatrists were required.
Follow-up Patient Management
Considering the risk of viral infection during recurrent hospital visits, patients under regular follow-up were advised to postpone follow-up visits and avoid returning to the hospital during the epidemic. During this period, patients were encouraged to maintain contact with their attending physicians through telephone or social networks to conduct a specific discussion on the review of their disease and possible discomfort. Tele-health consultations through certain apps on smartphone were also implemented.
Conclusion
At present, the epidemic of COVID-19 in Wuhan and other cities in Hubei Province has been temporarily controlled. Given the urgency of the diagnosis and treatment of malignant tumors, our cancer institute is gradually opening up (January 23, 2020, switch to state of emergency; March 21 open up; April 20 reach to full capacity) in an orderly manner. We hope that in the near future, the epidemic will eventually subside, allowing patients to be treated in a timely manner. We have endured much in the epidemic and also accumulated valuable experience in dealing with various issues. Based on the concept that life is priceless and all patients should be the center of our work, we were able to minimize the losses caused by the epidemic.
References
- Wu F, Zhao S, Yu B, et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579(7798):265-269.
- Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727-733.
- To KK, Tsang OT, Chik-Yan Yip C, et al. Consistent detection of 2019 novel coronavirus in saliva. Clin Infect Dis. 2020; ciaa149.
- Guan W-j, Ni Z-y, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708-1720.
- Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. J Amer Med Assoc. 2020;323(11):1061-1069.
- Liang W, Guan W, Chen R, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(3):335-337.
- Xiang YT, Yang Y, Li W, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiat. 2020;7(3):228-229.
- Strojan P, Vermorken JB, Beitler JJ, et al. Cumulative cisplatin dose in concurrent chemoradiotherapy for HN cancer: a systematic review. Head Neck. 2016;38Suppl1: E2151-2158.
- National Health Commission of China. New coronavirus pneumonia prevention and control program (4th ed). Jan 22, 2020. Accessed February 4, 2020, in Chinese. http://www. gov.cn/zhengce/zhengceku/2020-01/28/5472673/ les/0f96c10cc09d4d 36a6f9a9f0b42d972b.pdf
- Yang J, Yue JB, Liu J, Yu JM. Repopulation of tumor cells during fractionated radiotherapy and detection methods (review). Oncol Lett. 2014;7(6):1755-1760.
- Chow LQM. Head and neck cancer. N Engl J Med. 2020;382(1):60-72.
- Tang LQ, Chen DP, Guo L, et al. Concurrent chemoradiotherapy with nedaplatin versus cisplatin in stage II-IVB nasopharyngeal carcinoma: an open-label, non-inferiority, randomised phase 3 trial. Lancet Oncol. 2018;19(4):461-473.
- Sun XS, Liu SL, Liang YJ, et al. The role of capecitabine as maintenance therapy in de novo metastatic nasopharyngeal carcinoma: a propensity score matching study. Cancer Commun (Lond). 2020;40(1):32-42.
- Chua D, Wei WI, Sham JS, Au GK. Capecitabine monotherapy for recurrent and metastatic nasopharyngeal cancer. Jpn J Clin Oncol. 2008;38(4):244-249.
- Dada R, El Sayed M, Zekri J. Neoadjuvant chemotherapy with capecitabine plus cisplatin in patients with locally advanced nasopharyngeal cancer: case series study. J Glob Oncol. 2017;3(5):455-458.
- Zhang S, Zhou L, Huang X, Lin S. A retrospective study of concurrent chemoradiotherapy plus S-1 adjuvant chemotherapy on curative effect for treatment of patients with N3 stage nasopharyngeal carcinoma. Cancer Manag Res. 2018;10:1705-1711.
- Zong J, Xu H, Chen B, et al. Maintenance chemotherapy using S-1 following definitive chemoradiotherapy in patients with N3 nasopharyngeal carcinoma. Radiat Oncol. 2019,14(1):182.
- Peng PJ, Cheng H, Ou XQ, et al. Safety and efficacy of S-1 chemotherapy in recurrent and metastatic nasopharyngeal carcinoma patients after failure of platinum-based chemotherapy: multi-institutional retrospective analysis. Drug Des Devel Ther. 2014;8:1083-1087.
- Schiffer CA, Mangu PB, Wade JC, et al. Central venous catheter care for the patient with cancer: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol. 2013;31(10):1357-1370.
Citation
Wu Q, Yang X, Wu F, Zhong Y. Management of Head and Neck Cancer Patients During the Epidemic of COVID-19 in Wuhan. Appl Rad Oncol. 2020;(2):10-14.
June 22, 2020
