Formalized Mentorship in Radiation Oncology in the COVID Era: American College of Radiation Oncology Experience
Images


Abstract
Background: Formal mentorship in radiation oncology can create opportunities and promote career advancement, job satisfaction, and professionalism. Here, we report the results of the American College of Radiation Oncology (ACRO) Mentorship Program 2020-2021.
Methods: The ACRO Mentorship Program is advertised by email and social media, and dyad pairing occurs on a rolling basis every 2 weeks. We encourage participation from private practice, academic practice, and international applicants. A survey to assess program effectiveness was emailed to all participants in February 2021, and the results were analyzed.
Results: Seventy-eight individuals enrolled in the mentorship program: 40 to become a mentor, 50 to become a mentee; 12 individuals were interested in both. The survey response rate was 42.3%, and 66.7% believed that a formal mentorship is more beneficial compared with informal opportunities. The most common methods of mentor-mentee communication were via email (54.5%), video call (51.5%) and phone (45.5%). Survey respondents noted mutual respect, personal connection, shared values, and clear expectations in the mentor-mentee relationship. Participants felt mentors modeled professional and ethical behavior, taught new skills, and advised on career advancement and work-life integration. The majority of respondents (60.6%) desired to continue their mentor-mentee relationship beyond the formally required 1 year.
Conclusion: Formal mentorship programs remain a successful intervention in the COVID era and may be more beneficial compared with informal opportunities.
Keywords: Radiation oncology, mentorship, American College of Radiation Oncology
Mentorship is a critical component of medicine and can help with career advancement, job satisfaction, reinforcing ethics, and professionalism.1-4 Mentorship opportunities range from informal to formal, and participation can be either voluntary or mandatory.5 Informal mentorship can develop naturally from professional relationships and is frequently built upon mutual interests. Formal mentorship further extends opportunities to mentees who might not be able to secure a mentor within their own institution.6 Radiation oncology (RO) is a small specialty, and mentorship is important for career advancement.7 Medical students, specifically, may be at institutions without RO departments, making RO mentorship opportunities difficult to establish. In addition, as discussed by Seldon et al, it is often more difficult for women to find a female RO mentor.8 By helping to fill these gaps, formal mentorship programs may plan an important role in our field.
The American College of Radiation Oncology (ACRO) has been offering a dyad mentorship opportunity9 to medical students, residents, and new practitioners since 2015.10 In this program, mentors and mentees communicate via virtual platforms and can meet in-person at national meetings, such as the ACRO annual meeting. In this paper, we report the results of the ACRO Mentorship Program 2020-2021 and investigate its effectiveness in the era of COVID-19, which poses unique challenges for mentorship programs including physical distancing, financial losses, and competing priorities.11
Methods and Materials
The ACRO Mentorship Program starts in June and officially ends in May, spanning the academic year. The program is advertised on the ACRO website, by email, Twitter, personal referrals, and during the ACRO annual meeting. The ACRO Resident Committee sends out flyers to programs and highlights the mentorship program as a benefit of ACRO membership. The only requirement to enroll in this program is to fill out a form on the ACRO website, which collects demographic and geographic information, level of training, and specific personal requests. Pairing occurs on a rolling basis that happens every 2 weeks. Medical students, interns, residents, new practitioners, academic faculty, and private practice physicians can apply. Pairing is based on mentor and mentee requests. In addition, the program receives support from the ACRO resident and new practitioner committees to find appropriate mentors. Reminders are sent to mentor-mentee pairs before national meetings to encourage the mentor-mentee relationship and consideration of an in-person meeting.
>A survey to assess program effectiveness was designed and sent to all participants in February 2021. The anonymous survey was modeled after the Society of Women in Radiation Oncology (SWRO) mentorship questionnaire (see survey in Supplemental Material available online).8 Internal review board (IRB) exemption was obtained from Indiana University. All participants received an email with the Google Form survey link. The baseline characteristics and survey results were analyzed using JMP Pro 15 (SAS Institute Inc.). Chi-squared test was used and a P-value less than 0.05 was considered statistically significant.
Results
In the study period (June 2020 to May 2021), 78 individuals enrolled in the mentorship program: 28 to become a mentor, 38 to become a mentee; 12 individuals were interested in both. Therefore, there were 40 mentors and 50 mentees in the program. Baseline characteristics of mentorship program participants are summarized in Table 1. The mentor group consisted of radiation oncology residents (47.5%), academic faculty (40%) and private practice physicians (12.5%). Among resident mentors, 58% were junior (postgraduate year, PGY 1-3) and 42% were senior (PGY 4-5) residents. More than half of the mentors were males (57.7%), and 5% self-identified with the LGBTQI+ community. Geographic distribution of mentors was: 40% midwest, 27.5% south/southeast, 15% northeast, 12.5% west coast, and 5% international. Within the mentee group, 50% were residents, followed by medical students (46%) and new practitioners (4%). Half of the mentees were male and 2% associated with the LGBTQI+ community. Geographic distribution was: 32% midwest, 22% south/southeast, 36% northeast, 2% west coast, and 8% international. The distribution of mentors across residency training years was: 60% junior (PGY1-3) and 40% senior (PGY4-5).
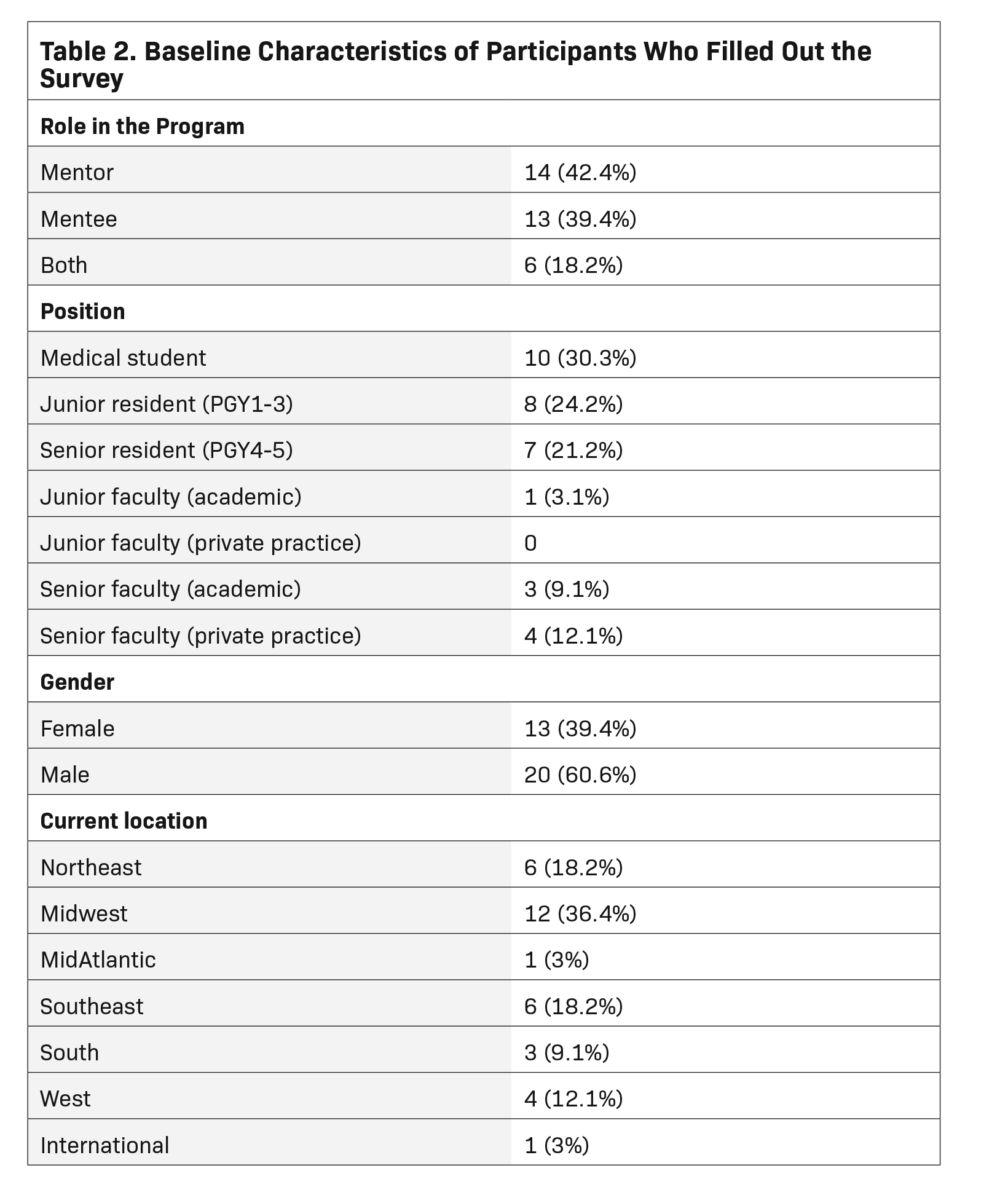
There was a 42.3% overall response rate to the survey: 14 mentors, 13 mentees, and 6 both. Therefore, the response rate was 50% (20/40) in the mentor group and 38% (19/50) in the mentee group. Table 2 summarizes the baseline characteristics of survey respondents. For 72.7% of the participants, this was their first year in the ACRO mentorship program. The survey showed that the most common method of communication between mentors and mentees was email (54.5%), followed by video call (51.5%) and phone (45.5%). Finally, 24.2% had the opportunity to meet in-person despite COVID pandemic restrictions.
Before initiating mentorship, 51.5% had no expectation about the number of interactions. However, 57.6% had at least 2 scheduled interactions since being paired. The pairs also managed to communicate outside scheduled interactions in 72.7% of cases. Either mentors or mentees set up the interactions in 54.5% of pairs, with mentees alone being responsible in 27.3% of pairs.
The survey considered different domains from which the mentor-mentee pairs benefited (Table 3). Mentees believed that mentors modeled professional and ethical behavior, taught them a new skill or knowledge, and advised on career advancement and work-life integration. Mentees also thought this relationship helped them promote networking. Mentors also answered the same questions about how they thought the relationship helped their mentees. Mentors believed they had more influence on direct and indirect job/ residency placement(P = 0.0001 and P = 0.007, respectively), research advice/collaboration (P = 0.001), advocating for mentee (P = 0.001), leadership advice (P = 0.001), modeling professional/ethical behavior (P = 0.004), and writing an editorial/serving as a discussant (P = 0.0005), compared with what mentees believed.
Mentors reported experiencing mutual respect (95.2%), a personal connection (66.7%), clear expectations (42.9%), and shared values (38.1%). Mentees similarly reported mutual respect (94.7%), shared values (73.7%), a personal connection (57.9%) and clear expectations (47.7%). A small minority of mentors reported lack of experience (9.5%) and lack of commitment (5.3%) in mentees, but mentees did not have the same concerns about the mentors.
style="padding-left: 5pt;text-indent: 9pt;text-align: justify;">Among the survey respondents, all participants had expressed having additional mentorship relationships beyond the ACRO program. Most (66.7%) believed that a formal mentorship is more beneficial compared with informal opportunities, while 30% felt both mentorship types are equally beneficial. Finally, 60.6% of participants were very satisfied with their pairing and would like to continue their mentorship relationship beyond the formal 1-year duration of the program.
Discussion
Our study showed that a formal mentorship program in the COVID era continues to be a successful paradigm, with participants reporting the strategy to be more beneficial compared with informal opportunities. The benefits of a formal mentorship program and participants’ experience include mutual respect, personal connection, a shared value set, and clear expectations. This study also showed that mentor and mentee interpretation of relationship and benefit aspects can vary. In certain aspects, such as advocacy, job/residency placement and writing an editorial/serving as the discussant, the mentee might not be aware of the role of mentor in these domains. However, in other aspects, such as leadership and research advice, mentors may need to communicate more clearly with mentees.
The ACRO Mentorship Program has mentors currently in private practice (12.5% of the mentor group). As 60% of radiation oncologists work in private practice,12 it is important to find ways to encourage more involvement of this group in mentorship programs. In addition, this year we were able to expand the program to provide mentorship opportunities internationally, in both mentor (5%) and mentee groups (8%). There were students and graduates enrolled in our program who were interested in pursuing training in the US and were seeking mentors with a similar background. Finally, we received a few requests (3.8% in the overall mentor/mentee pool) from the LGBTQI+ community and were able to provide better support by finding them a mentor/mentee from the LGBTQI+ community. Based on our experience from last year, we have updated our registration form to be more inclusive with respect to the background of our participants to fulfill their requests with the goal of a higher satisfaction rate and a more meaningful relationship.
In a recent publication by Marsiglio et al, 13 papers on mentorship in radiation oncology were reviewed.9 Similar to the ACRO program, the dyad mentorship was found to be the most reported type of mentorship. This review also demonstrated that participants were more satisfied with formal mentorship compared with informal mentorship, as found in our study. Additionally, achieving career goals and work- life balance were among the benefits of the mentorship program participation, which is similar to our findings. However, the participants in the ACRO Mentorship program also felt that the relationship helped them model professional and ethical behavior. Our study showed a higher satisfaction rate, with 60.6% of participants wishing to continue their relationship, compared with 35.7% in the review.9 This might be due to the larger and heterogenous pool of participants in the Marsiglio et al study. In addition, participants can share their specific requests and interests on the ACRO Mentorship Program registration forms, and ACRO committee members work to honor these requests when possible.
With advancements in technology as well as the ongoing COVID pandemic, virtual platforms are now used as one of the main methods of communication in mentorship programs.13 In our ACRO mentorship program, 51.5% used video calls to communicate. As discussed by Seldon et al, SWRO has also used digital mentorship.8 The virtual platform has enabled the ACRO Mentorship Program to engage participants from different states and countries and is likely an important contributor to the continued success of the mentorship program in the COVID era. The American Society of Radiation Oncology (ASTRO) mentorship match program reported results at the 2017 ASTRO annual meeting. There was no virtual option for this program; 64% of residents and 73% of attendings preferred in-person meetings, and only 21% of residents expressed interest in a mentorship program utilizing social media.10 Participants’ preferences have changed over time, which may be related to increased comfort with virtual platforms in the COVID era. Social media may also have more application in current mentorship models. With more programs turning toward virtual platforms and social media, it is possible to connect mentors and mentees from different institutions and allow them to develop a mentorship relationship.
This study has its own limitations. Longer follow-up will be beneficial to better assess the long-term benefits of the mentorship program. We only assessed the short-term benefits of a formal mentorship program. Based on Kashiwagi et al systemic review results,14 future programs can also investigate providing goal setting and career planning worksheets to better guide the relationship since our study showed that less than half of the participants had clear expectations about their relationship. Another limitation of this study is the low rates of participation from private practice (12.5%). In addition, we had a modest response rate with 42.3% of participants sharing their experience. Finally, we did not collect comprehensive demographic data regarding race/ethnicity and were unable to meaningfully assess diversity and our program’s ability to assist underrepresented minorities.
Conclusion
The ACRO Mentorship Program provided formal RO mentorship opportunities and resulted in high rates of participant satisfaction despite challenges of the COVID era. This program will continue to engage participants from all scopes of practice (academia and private practice), diverse backgrounds, and underrepresented RO groups such as women and will also continue to use virtual platforms in addition to in-person meetings to promote the mentor-mentee relationship.
References
- Choi AMK, Moon JE, Steinecke A, Prescott JE. Developing a culture of mentorship to strengthen academic medical centers. Acad Med. 2019;94(5):630-33 doi: 10.1097/ acm.0000000000002498
- Scandura TA. Mentorship and career mobility: an empirical investigation. J Organ Behav. 1992;13(2):169-174.
- Sambunjak D, Straus SE, Marusić A. Mentoring in academic medicine: a systematic review. JAMA. 2006;296(9):1103-15 doi:10.1001/jama.296.9.1103
- Wong RK, Vanderpuye V, Yarne J, et al. Clinical research mentorship programme (CRMP) for radiation oncology residents in Africa–building capacity through mentoring. Ecancermedicalscience. 2021;15:1210 doi:10.3332/ecancer.2021.1210
- Goldinger G, Nesher L. Mind the gap, factors that affect mentee’s satisfaction in a formal mentorship program with arbitrary matching. MedEdPublish. 2021;10(1):49.
- Lonnie D, Inzer CC. A review of formal and informal mentoring: processes, problems, and design. J Leader Ed. 2005;4(1).
- Holliday EB, Jagsi R, Thomas CR, Wilson LD, Fuller CD. Standing on the shoulders of giants: results from the Radiation Oncology Academic Development and Mentorship Assessment Project (ROADMAP). Int J Radiat Oncol Biol Phys. 2014;88(1):18-24 doi:10.1016/j.ijrobp.2013.09.035
- Seldon C, Wong W, Jagsi R, Croke J, Lee A, Puckett L. Remote mentorship in radiation oncology: lessons to share. Adv Radiat Onc. 2021;6(4):100686 doi:10.1016/j. adro.2021.100686
- Marsiglio JA, Rosenberg DM, Rooney MK, et al. Mentorship initiatives in radiation oncology: a scoping review of the literature. Int J Radiat Oncol Biol Phys. 2021;110(2):292- 302 doi:10.1016/j.ijrobp.2020.12.049
- Engel S, Lischalk JW, Barry P, et al. Radiation oncology resident mentorship: results of a resident-coordinated mentorship program. J Amer Coll Radiol. 2017;14(12):1607- 1610. doi:10.1016/j.jacr.2017.07.011
- Perry RE, Parikh JR. COVID-19: a call for mentorship in radiology. Clin Imag. 2021;79:48-51. doi:10.1016/j.clinimag.2021.04.003
- Fung CY, Chen E, Vapiwala N, et al. The American Society for Radiation Oncology 2017 Radiation Oncologist Workforce Study. Int J Radiat Oncol Biol Phys. 2019;103(3):547- 556. http://doi.org/10.1016/j.ijrobp.2018.10.020
- Gottlieb M, Fant A, King A, et al. One click away: digital mentorship in the modern era. Cureus. 2017;9(11):e1838 doi:10.7759/cureus.
- Kashiwagi DT, Varkey P, Cook DA. Mentoring programs for physicians in academic medicine: a systematic review. Acad Med. 2013;88(7):1029-1037. doi:10.1097/ ACM.0b013e318294f368
Citation
Arbab M, Chaurasia A, Merfeld E, Hassanzadeh C, Sherer MV, Razavian N, Schutz A, Sandoval M, Holmes JA, Puckett L, Dragun JB, Schuster J. Formalized Mentorship in Radiation Oncology in the COVID Era: American College of Radiation Oncology Experience. Appl Rad Oncol. 2021;(12):18-24.
December 28, 2021
